When you take vitamin D to support bone health and immune function, and your doctor prescribes a thiazide diuretic for high blood pressure, you might think you're doing everything right. But here's the hidden risk: combining these two can push your blood calcium levels into dangerous territory. It's not rare. It's not theoretical. It's happening to thousands of people right now - often without anyone realizing why.
Thiazide diuretics like hydrochlorothiazide (Microzide) and chlorthalidone are among the most commonly prescribed blood pressure medications in the U.S., with over 50 million prescriptions filled each year. They work by helping your kidneys get rid of extra salt and water. But there's a side effect most people don't know about: they cause your body to hold onto calcium instead of flushing it out in urine. That sounds harmless - until you add vitamin D into the mix.
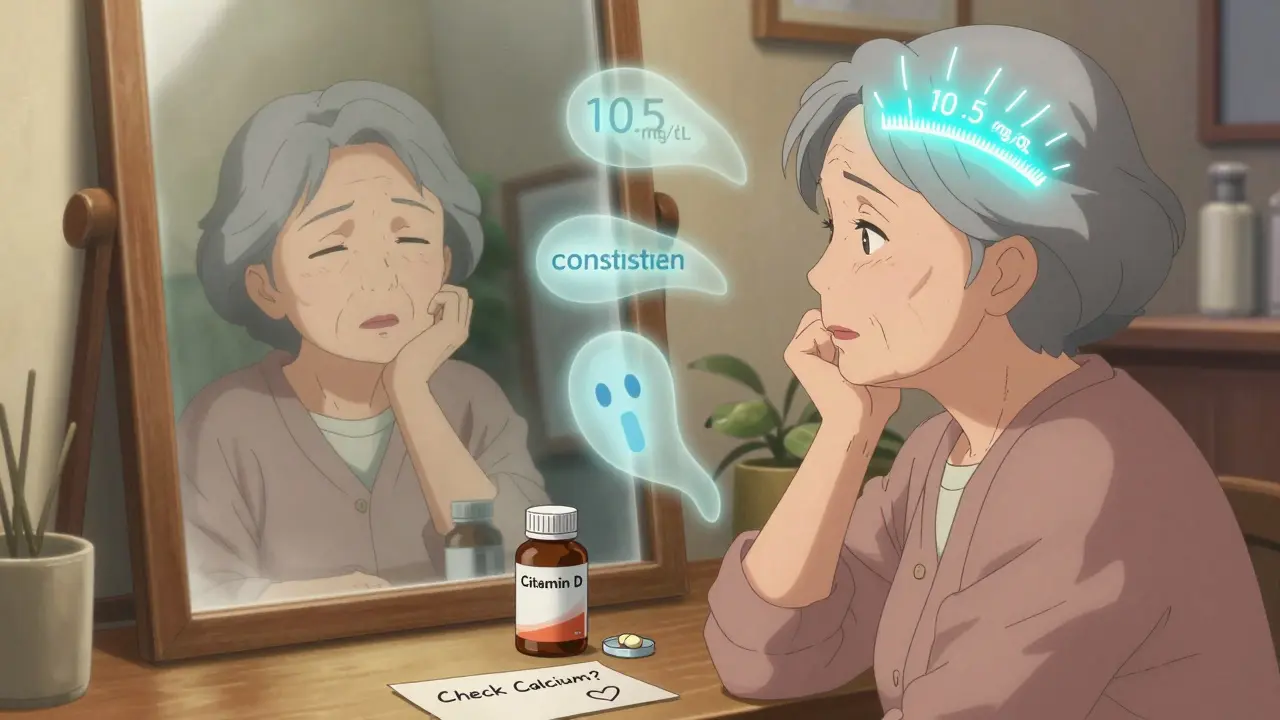
Vitamin D, especially in doses above 2,000 IU daily, makes your intestines absorb way more calcium from food. When that happens on top of a thiazide's calcium-retaining effect, your body can't handle the overload. Your blood calcium levels creep up. And when they hit above 10.5 mg/dL, you're in hypercalcemia territory. Symptoms? Fatigue, nausea, constipation, confusion, frequent urination, even kidney stones. In older adults, it can lead to hospitalization.
How the Two Work Together - And Why That's Dangerous
Let’s break it down simply. Your kidneys normally filter calcium and let some pass out in urine. Thiazide diuretics block a specific transporter in the kidney called the NCC. That reduces sodium loss - good for lowering blood pressure - but it also tricks the kidney into reabsorbing more calcium. Studies show this cuts urinary calcium excretion by 30-40%. That means more calcium stays in your bloodstream.
Meanwhile, vitamin D - specifically its active form, calcitriol - turns on proteins in your gut that pull calcium from your food into your blood. At high doses (5,000 IU or more), this can increase calcium absorption by up to 80%. So you're not just getting more calcium from your diet; your kidneys are also holding onto every bit of it.
This isn't just a theory. A 2021 study from the Mayo Clinic found that people taking more than 4,000 IU of vitamin D daily while on a thiazide had an 8-12% chance of developing hypercalcemia. Compare that to just 2-3% for those on thiazides alone. And according to the National Hospital Ambulatory Medical Care Survey, 15% of all emergency visits for drug-induced hypercalcemia involved this exact combo.
Who’s at Highest Risk?
It’s not everyone. But certain groups are far more vulnerable:
- Older adults - Over 65, especially those on multiple medications. A 2023 JAMA study found 22% of hypercalcemia cases in seniors were tied to this interaction.
- People taking high-dose vitamin D supplements - Many take 5,000 IU, 10,000 IU, or even more thinking “more is better.” The Endocrine Society recommends only 600-800 IU daily for most adults.
- Those with borderline calcium levels - If your baseline calcium was already near 10.2 mg/dL, adding vitamin D and a thiazide can push it over the edge.
- People with kidney issues - Even mild kidney changes reduce your body’s ability to clear excess calcium.
A 2022 survey by the National Council on Aging found that 61% of seniors on thiazides had no idea they needed to check their calcium levels when taking vitamin D. That’s not negligence - it’s a gap in communication.
What About Other Diuretics?
Not all water pills are the same. Loop diuretics like furosemide (Lasix) actually make you lose more calcium - so they don’t carry this risk. Potassium-sparing diuretics like spironolactone don’t affect calcium much either. That’s why some doctors switch patients from thiazides to these alternatives if they need high-dose vitamin D.
But thiazides are still the go-to for most primary care doctors - 68% prefer them - because they control blood pressure better over 24 hours than alternatives. The problem? The benefits come with a hidden cost. And many clinicians still don’t monitor for it.
What Should You Do?
If you’re on a thiazide diuretic and taking vitamin D, here’s what you need to do right now:
- Check your current vitamin D dose. If it’s over 2,000 IU daily, talk to your doctor. Most people don’t need more than 800-1,000 IU.
- Ask for a serum calcium test. It’s a simple blood test. Do it now if you haven’t had one in the last 6 months. If your calcium is above 10.2 mg/dL, this interaction is likely playing a role.
- Consider alternatives. If you’re on hydrochlorothiazide 25 mg, ask if you can switch to 12.5 mg - it’s often just as effective for blood pressure but with less calcium retention.
- Monitor symptoms. Unexplained fatigue, constipation, frequent urination, or brain fog? These aren’t just “getting older.” They could be early signs of high calcium.
Pharmacist-led programs have cut hypercalcemia rates in half by simply setting up routine calcium checks. One 2022 study in the Journal of Clinical Pharmacy and Therapeutics showed a drop from 11.3% to 2.7% in patients who got regular monitoring. That’s not magic - it’s basic care.
What’s Changing in Guidelines
The medical community is waking up. The American Society of Nephrology now recommends testing calcium levels every 3-6 months for anyone on this combo. The European Society of Cardiology says never exceed 2,000 IU/day of vitamin D if you’re on a thiazide. The American Geriatrics Society lists this combination as potentially inappropriate for older adults with already elevated calcium.
And it’s not just guidelines - technology is catching up. Kaiser Permanente now uses electronic health record alerts that pop up when a patient on a thiazide gets prescribed vitamin D over 2,000 IU. Since launching this in 2021, they’ve reduced dangerous combinations by 63%.
Even the FDA updated thiazide drug labels in 2021 to include hypercalcemia warnings. And in 2023, a new diagnostic test called CalcCheck was approved - it looks at your genes to predict how likely you are to develop high calcium from this interaction.
The Bottom Line
You can still take vitamin D. You can still take your blood pressure pill. But you can’t take them together without awareness. This isn’t about stopping either one. It’s about managing them smartly.
For most people, 800-1,000 IU of vitamin D daily is enough. For those on thiazides, that’s the sweet spot - enough to support bone health without tipping calcium into danger. Higher doses? Only if you’re under close supervision, with regular blood tests.
The benefits of controlling high blood pressure with thiazides are real. The risks of unchecked hypercalcemia are real too. But here’s the good news: this risk is entirely preventable. All it takes is a simple blood test and a conversation with your doctor.
Don’t wait until you feel sick. Don’t assume your doctor already knows. Ask: “Could my vitamin D and blood pressure pill be affecting my calcium?” That one question could save you from a hospital trip.
Can vitamin D and thiazide diuretics cause high calcium levels?
Yes. Thiazide diuretics reduce calcium loss in urine, while vitamin D increases calcium absorption from food. Together, they can cause serum calcium levels to rise above 10.5 mg/dL - the clinical threshold for hypercalcemia. Studies show this combination raises the risk from 2-3% to 8-12% in people taking high-dose vitamin D (over 4,000 IU/day).
How much vitamin D is safe with a thiazide diuretic?
For most people on thiazides, 800-1,000 IU per day is considered safe. The Endocrine Society recommends this range for adults. Doses above 2,000 IU/day significantly increase hypercalcemia risk, and the European Society of Cardiology advises against exceeding this limit. Always check your calcium level before starting or increasing vitamin D.
Do all diuretics increase calcium levels?
No. Only thiazide and thiazide-like diuretics (like chlorthalidone and indapamide) reduce calcium excretion. Loop diuretics like furosemide increase calcium loss in urine, making them safer for people taking vitamin D. Potassium-sparing diuretics like spironolactone have little to no effect on calcium.
How often should I get my calcium checked if I’m on both?
The American Society of Nephrology recommends testing serum calcium within 3 months of starting the combination, then every 6-12 months. If you’re over 65, have kidney issues, or take more than 2,000 IU of vitamin D daily, testing every 3-6 months is advised. Many primary care doctors still don’t follow this - so ask for it.
What are the symptoms of hypercalcemia from this interaction?
Symptoms include fatigue, nausea, constipation, increased thirst, frequent urination, confusion, muscle weakness, and bone pain. In older adults, these are often mistaken for normal aging. A 2023 study found that 78% of patients on this combo reported fatigue - and didn’t connect it to their meds. If you notice these symptoms, get your calcium tested.
Can I switch to a different blood pressure pill to avoid this?
Yes. If you need high-dose vitamin D, your doctor may switch you to a loop diuretic like furosemide or a potassium-sparing diuretic like spironolactone. These don’t retain calcium. However, thiazides are often preferred for long-term blood pressure control. The decision depends on your overall health, kidney function, and blood pressure goals.
Is this interaction more common in older adults?
Yes. Over 80% of adults over 65 take at least one of these medications. A 2023 Mayo Clinic study found that 22% of hypercalcemia cases in seniors were caused by this interaction. Many older adults take vitamin D supplements without knowing the risk, and their kidneys are less able to clear excess calcium. This makes them especially vulnerable.
Are there any tests to predict my risk?
Yes. In 2023, the FDA approved a genetic test called CalcCheck that analyzes variants in the calcium-sensing receptor gene (CASR). People with certain variants are 3-4 times more likely to develop hypercalcemia on this combo. While not yet routine, it’s becoming available in specialty clinics and may soon be part of standard care for high-risk patients.
