If you’re on Medicaid and need prescription drugs, you might assume your meds are fully covered. But that’s not always true. Medicaid pays for most prescription medications-but not all. And even when they do, you could still face copays, prior authorizations, or even be told you have to try cheaper drugs first. This isn’t about confusion-it’s about how the system actually works in 2025.
What Medicaid Actually Covers
All 50 states and D.C. cover outpatient prescription drugs under Medicaid. That’s not optional-it’s standard. But here’s the catch: each state decides which drugs are covered and under what rules. There’s no single national list. Instead, every state runs its own Preferred Drug List (PDL), which acts like a pharmacy menu. These lists are updated regularly-sometimes multiple times a year.
Most Medicaid plans group drugs into tiers. Tier 1 usually includes generics-low-cost, high-value meds like metformin for diabetes or lisinopril for high blood pressure. These often come with a $1-$5 copay. Tier 2 is for brand-name drugs that don’t have a generic version yet. These cost more-maybe $10-$30. Tier 3 and above? That’s where specialty drugs live: things like insulin pens, hepatitis C cures, or rheumatoid arthritis biologics. These can cost hundreds, even thousands, per month. Medicaid covers them, but only if you jump through hoops.
According to CMS data, generics make up 89% of all Medicaid prescriptions-but only 27% of the total spending. Meanwhile, just 3% of prescriptions are for specialty drugs, yet they account for 42% of costs. That’s why states are so strict about controlling access to them.
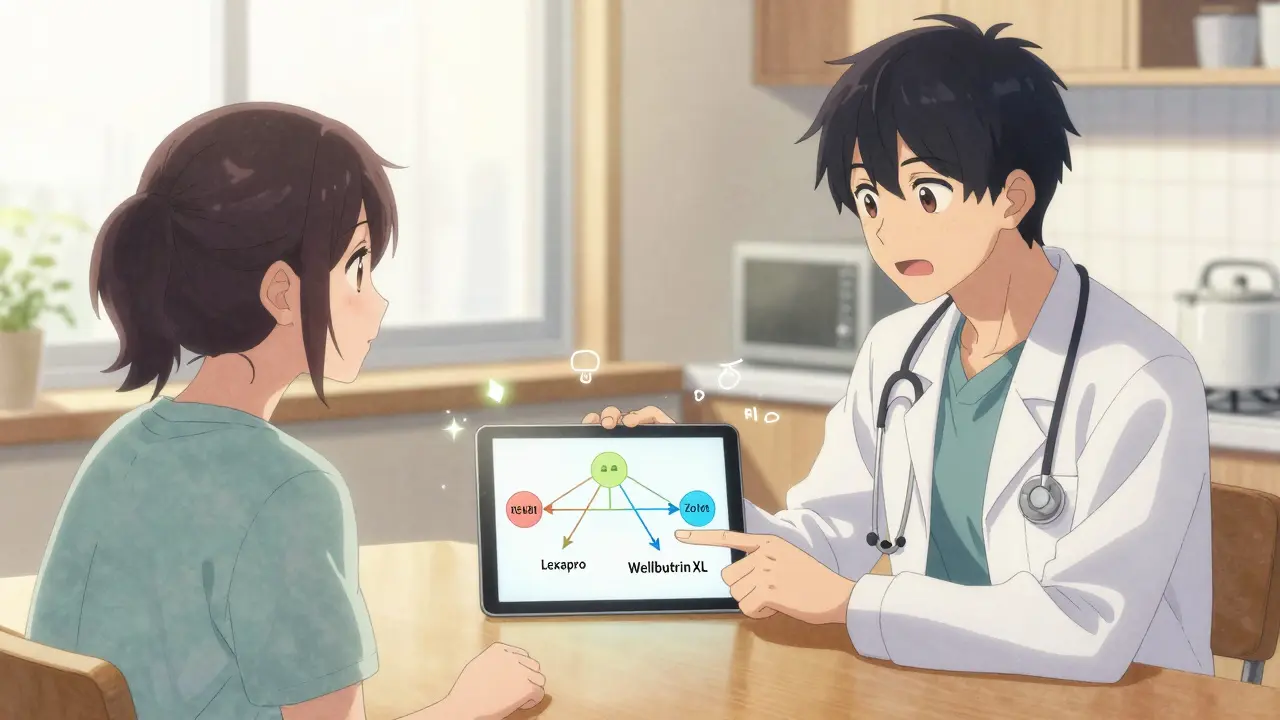
Step Therapy: You Have to Try Cheaper Drugs First
One of the most common roadblocks is called step therapy, or “trial and failure.” It means you can’t get the drug your doctor prescribed unless you’ve tried-and failed-two other, cheaper drugs first.
For example: your doctor prescribes Wellbutrin XL for depression. But your state’s PDL lists Lexapro and Zoloft as preferred. You have to take Lexapro for 6-8 weeks. If it doesn’t work, you try Zoloft. Only after both fail can you get Wellbutrin approved. This isn’t just paperwork-it’s real time lost. The Medicare Rights Center found that 63% of Medicaid users experienced delays because of step therapy. Some waited over two weeks just to get a decision.
North Carolina, for instance, requires two failed trials for most drug classes. Florida does too. But some states are more flexible, especially for mental health or rare diseases. The problem? Many patients don’t know this rule exists until they’re denied at the pharmacy counter.
Prior Authorization: The Paperwork Maze
Even if a drug is on the formulary, you might still need prior authorization. This means your doctor has to submit a request to Medicaid-often with lab results, diagnosis codes, and proof that other drugs didn’t work. The form can be 5 pages long. Some states require it for insulin, asthma inhalers, or even birth control.
North Carolina requires prior authorization for certain insulin types, like premixed rapid combination insulin, but only if it’s for Type 1 Diabetes-and even then, the approval can last up to three years if the clinical case is solid. That’s a rare exception. Most approvals last 6-12 months, meaning you have to reapply every year.
Here’s what most people don’t realize: 78% of denied prior authorizations get approved on appeal-if the doctor submits full clinical notes. That’s not luck. That’s knowing the system. If your request is denied, don’t give up. Ask your doctor to resubmit with more detail.
Costs You Still Pay
Medicaid doesn’t mean free. Copays vary by state and drug tier. In 2025, most states cap generic copays at $5 and brand-name at $12. But if you’re eligible for Extra Help (a federal program for low-income Medicare beneficiaries who also have Medicaid), your costs drop even further: $0 premium, $0 deductible, $4.90 for generics, $12.15 for brands. And once you hit $2,000 in annual drug spending, you pay nothing for the rest of the year.
But here’s the kicker: only about half of eligible people sign up for Extra Help. The Medicare Rights Center estimates 1.2 million people miss out because they don’t know they qualify. If you have full Medicaid coverage, you automatically qualify. You don’t need to apply separately. Call your state’s SHIP (State Health Insurance Assistance Program) office and ask: “Do I get Extra Help?”
What’s Not Covered
Some drugs are simply off-limits. States remove medications from their formularies for one reason: they don’t get a rebate from the manufacturer. In October 2025, North Carolina dropped 12 drugs-including Vasotec, Trulance, and Vanos Cream-because the drug companies stopped offering rebates. That doesn’t mean they’re unsafe. It means they’re too expensive for the state to afford under current rules.
Also excluded: over-the-counter meds (unless prescribed for a specific condition), weight-loss drugs like Ozempic (in most states), and fertility treatments. Some states cover smoking cessation aids like Chantix, others don’t. There’s no national standard.
How to Find Your State’s Formulary
You can’t guess what’s covered. You have to look it up. Every state publishes its Preferred Drug List online. Here’s how:
- Go to your state’s Medicaid website (search “[Your State] Medicaid formulary”)
- Look for “Preferred Drug List,” “Formulary,” or “Drug List”
- Download the PDF or use the searchable tool
- Search your medication by brand or generic name
- Check the tier, any restrictions (step therapy, prior auth), and expiration date
States update these lists frequently. North Carolina revised its formulary in July and October 2025. CVS Caremark, Express Scripts, and OptumRx-the pharmacy benefit managers that run Medicaid drug plans-also post updates. If you’re on Medicaid, check your formulary every 6 months. A drug that was covered last year might not be this year.
Network Pharmacies and Mail Order
You can’t just walk into any pharmacy. Medicaid only pays for prescriptions filled at in-network pharmacies. Most states partner with big chains like CVS, Walgreens, or Walmart. But some rural areas have limited options. That’s why many states push mail-order for maintenance meds (like blood pressure or diabetes pills). You can get a 90-day supply shipped to your door for the same price as a 30-day fill at the pharmacy.
Using mail order saves money-and reduces trips to the pharmacy. But you need to sign up through your Medicaid plan. Don’t assume it’s automatic. Call your plan’s pharmacy line and ask: “Can I get my maintenance drugs by mail?”
What’s Changing in 2025-2026
Two big changes are coming:
- Monthly drug changes: Starting in 2025, if you’re on Medicaid or Extra Help, you can switch your drug plan once a month-not just during the annual enrollment period. This is huge. If your medication gets pulled from the formulary, you can switch to a plan that covers it right away.
- New federal rules: In early 2026, CMS will require states to prove their formularies don’t block medically necessary drugs. That means states can’t just cut drugs for cost alone. They’ll have to show patients still have access to effective treatments. This could lead to more drugs being added back to lists.
Also, the Inflation Reduction Act’s $2,000 out-of-pocket cap for Medicare Part D now applies to dual-eligible beneficiaries (those on both Medicare and Medicaid). If you’re on both, your drug costs are now capped at $2,000 a year-no matter how expensive your meds are.
What to Do If You’re Denied
Being denied a drug doesn’t mean it’s gone forever. Here’s your action plan:
- Ask the pharmacist for the denial reason. Get it in writing.
- Contact your doctor. Ask them to submit a prior authorization appeal with clinical notes.
- Call your state’s SHIP hotline. They help for free. Find yours at shiphelp.org (no link needed in final output).
- File an appeal with your Medicaid plan. You have 60 days.
- If denied again, request a fair hearing. You have the right.
Don’t stop at the first no. Most denials are overturned with proper documentation.
Final Takeaways
- Medicaid covers most prescriptions-but not all. Check your state’s formulary every 6 months.
- Step therapy and prior auth are common. Be prepared to prove your meds are necessary.
- You still pay copays, but Extra Help can cut them to near zero.
- Mail-order pharmacies save money and hassle for long-term meds.
- If you’re denied, appeal. 78% of appeals succeed with good paperwork.
- Drug lists change often. What’s covered today might not be next month.
The system is complicated, but it’s not impossible. Knowing how it works gives you power. Don’t wait until you’re at the pharmacy counter to figure it out. Do your homework now. Your health depends on it.