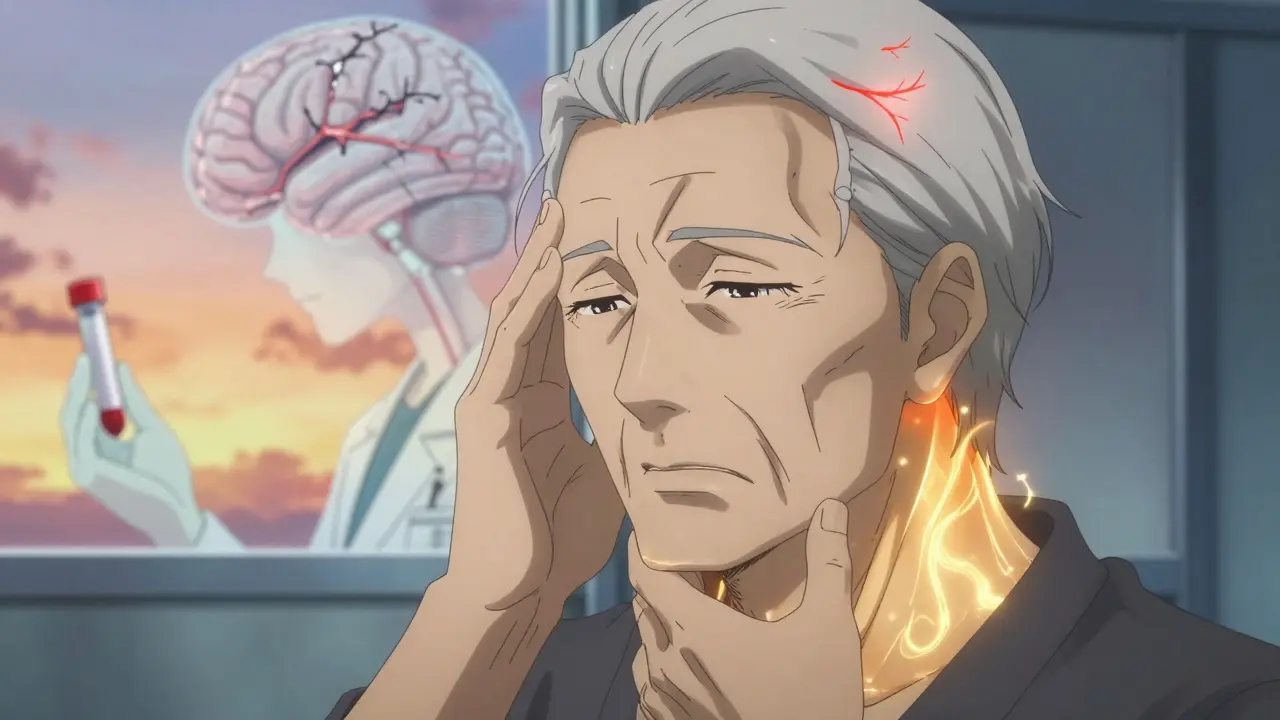
Most headaches are just a nuisance-maybe from stress, lack of sleep, or too much coffee. But sometimes, a headache isn’t just a headache. It could be your brain screaming for help. When a headache comes with certain warning signs, waiting even an hour could mean the difference between full recovery and permanent damage-or worse.
Thunderclap Headache: The Brain’s Emergency Signal
Imagine a headache that hits like a lightning strike. One second you’re fine, the next you’re on your knees, clutching your head, unable to think. That’s a thunderclap headache. It peaks within 60 seconds and feels like the worst headache of your life. This isn’t just bad luck-it’s a medical emergency.Eighty-five percent of subarachnoid hemorrhages-bleeding around the brain from a ruptured aneurysm-start this way. A 2021 study in Neurology found that if you ignore this symptom, your chance of rebleeding increases by 40% after just four hours. Even if a CT scan looks normal, you still need an MRI within four hours. Why? Because up to 5% of these bleeds don’t show up on the first scan. Hospitals like Mass General Brigham now require a non-contrast CT within 30 minutes of arrival. Delaying care isn’t just risky-it’s dangerous.
Neurological Symptoms: When Your Body Betrays You
Headaches that come with weakness, slurred speech, blurred vision, or confusion aren’t migraines. They’re red flags. These aren’t vague feelings-they’re clear signs your brain isn’t working right.Weakness on one side of your body? That’s a stroke in 63% of cases, according to the American Heart Association. Blurred or double vision? Could be pressure on your optic nerve or a brain tumor. Slurred speech? That’s not anxiety-it’s likely a stroke or other neurological event. A 2022 CDC study showed 78% of people with bacterial meningitis had altered mental status. And if you’re having trouble speaking or moving, you need to get to the ER within three hours. Every minute counts. The Get With The Guidelines-Stroke registry found 68% of these cases were strokes, and early treatment cuts disability risk by more than half.
Headaches After 50: Don’t Assume It’s Just Aging
If you’re over 50 and suddenly get a new kind of headache, don’t brush it off as stress or tiredness. This is one of the most under-recognized red flags. The risk of giant cell arteritis-a dangerous inflammation of blood vessels in the scalp and neck-goes up 23-fold after age 50. And if you have jaw pain when chewing, scalp tenderness, or vision changes along with the headache, it’s almost certainly this condition.Giant cell arteritis can cause blindness in hours if untreated. The 2023 European League Against Rheumatism guidelines say that when jaw claudication and temporal artery tenderness are present, the diagnosis is 94% specific. Yet, many doctors miss it because they don’t think of it in older patients. The American Academy of Neurology warns that new-onset headaches in people over 50 carry a 1 in 200 risk of brain tumor. Glioblastoma, the most aggressive type, makes up nearly half of these cases. A simple blood test (ESR and CRP) and urgent steroid treatment can prevent blindness and death.
Fever, Stiff Neck, and Headache: Meningitis Doesn’t Wait
If your headache comes with fever, stiff neck, and sensitivity to light, treat it like a fire alarm. This isn’t the flu. This could be meningitis-bacterial, fungal, or viral. Bacterial meningitis kills 17% of patients if untreated, and every hour of delay increases the death risk by 5.2%, according to the 2022 IDSA guidelines.Neck stiffness isn’t just soreness. It’s meningismus-when your body locks up because the lining around your brain is inflamed. In 92% of bacterial meningitis cases, this symptom appears with fever. The CDC says 78% of patients had altered mental status. That means confusion, drowsiness, or trouble waking up. If you see this combo, don’t wait for a doctor’s appointment. Go to the ER now. Antibiotics must be given within 45 minutes of triage. Delaying by just 30 minutes raises mortality by 7.2%. One Reddit user, 'HeadacheSurvivor89,' ignored their symptoms for four hours. They ended up with a ruptured aneurysm and permanent brain damage. Another user, 'NeuroAlert,' went straight to the ER when they got fever and neck stiffness. They had viral meningitis-and early treatment kept them out of the ICU.

Head Injury and Headache: When the Blow Is Worse Than It Seems
A bump on the head isn’t always harmless. If you’ve had a head injury and now have a headache, watch for more than just pain. Loss of consciousness for more than five minutes? Vomiting more than twice? Confusion or memory loss? These are red flags that mean you could have a brain bleed.The 2022 PECARN guidelines show that vomiting twice after trauma has a 68% positive predictive value for intracranial hemorrhage. A drop of two or more points on the Glasgow Coma Scale? That’s a sign your brain is swelling. The NEXUS II criteria say you need a CT scan within one hour. In rural areas, where neurologists aren’t available 24/7, patients wait an average of 3.2 hours for care. That delay can turn a treatable bleed into a fatal one. Even if you feel okay at first, symptoms can worsen over hours. Don’t wait. If you hit your head and then feel off, get checked.
Immunosuppression and Headache: A Silent Killer
If you’re on chemotherapy, have HIV, take steroids long-term, or had an organ transplant, your body can’t fight off infections like it used to. That means even a simple headache can be a sign of fungal meningitis-a rare but deadly condition.The American College of Emergency Physicians says immunosuppressed patients with any new headache need immediate evaluation. Why? Fungal meningitis has a 35% mortality rate-even with treatment. The CDC’s VAERS data shows 0.8 cases per 100,000 mRNA vaccine doses, but the real danger is in people with weakened immune systems. In one case, a patient with lupus on immunosuppressants had a mild headache for three days. They thought it was allergies. By day four, they were in a coma. Fungal meningitis doesn’t always cause fever. Sometimes, it just starts with a headache that won’t go away. If you’re immunocompromised, don’t guess. Go to the ER.
Progressive Headaches: The Slow Burn That Turns Deadly
Some headaches don’t hit like a bomb-they creep in. If your headache gets worse over days or weeks, especially if it’s worse in the morning or wakes you up at night, that’s a red flag. This pattern often means a brain tumor or increased pressure inside the skull.Studies show 74% of patients with intracranial masses have progressive headaches. The pain may get worse with bending over, coughing, or lying down. You might also notice nausea, vomiting, or vision changes. Papilledema-swelling of the optic nerve-is a key sign. The American College of Radiology now recommends MRI over CT for these cases because it’s 22% more sensitive at detecting early pressure changes. A 2023 study in JAMA Internal Medicine found that using the AAN’s Red Flag Headache Decision Tree correctly identified 94% of secondary headaches while cutting unnecessary scans by 37%. Don’t assume it’s tension or migraines if it’s getting steadily worse.
What to Do When You See the Red Flags
You don’t need to be a doctor to know when to act. Here’s the simple rule: If your headache comes with any of these, call 911 or go to the ER immediately:- It hits like a thunderclap-peaks in under a minute
- You have weakness, numbness, slurred speech, or vision loss
- You’re over 50 and this is a new kind of headache
- You have fever + stiff neck + confusion
- You had a head injury and now feel worse
- You’re immunocompromised and have any new headache
- The headache keeps getting worse over days
Don’t text your doctor. Don’t wait to see if it gets better. Don’t assume it’s stress. Emergency departments use the SNOOP4 tool to screen for these signs in under 10 minutes. If you’re unsure, err on the side of caution. The American Headache Society’s campaign says it best: “If your headache comes with confusion, weakness, or vision changes, don’t wait-call 911 immediately.” And they’re right. A 2023 survey found 78% of people who acted fast avoided permanent disability. Only 32% of those who waited did.
Why People Miss the Signs
The National Headache Foundation surveyed 1,247 people. Sixty-three percent ignored their symptoms at first. Twenty-eight percent waited more than six hours before seeking help. Why? Because headaches are common. Because they think it’s just a migraine. Because they don’t know the difference between a bad headache and a brain emergency.One patient on HealthUnlocked, 'MigraineWarrior,' had blurred vision and slurred speech. Their ER visit was delayed by 3.5 hours because they were told it was anxiety. They had a stroke at 32. Permanent vision loss. That’s not rare. It’s preventable.
Doctors miss these signs too. Misdiagnosis rates for serious headaches are 15-20% when red flags are overlooked. And in rural areas, where specialists aren’t available, delays are longer. The American Academy of Neurology says failure to recognize thunderclap headache is one of the top three reasons neurologists get sued. That’s not just statistics-it’s real people losing their lives because someone didn’t act.
Final Thought: Trust Your Instincts
Your body knows when something’s wrong. If a headache feels different-worse, faster, stranger-listen to it. You don’t need to understand neurology to know when something’s off. If you feel like something is seriously wrong, you’re probably right. Don’t wait for someone else to confirm it. Don’t let fear of overreacting stop you from saving your life.Is a thunderclap headache always a sign of a brain bleed?
Not always, but it’s the most common warning sign of a subarachnoid hemorrhage. About 85% of these bleeds start with a thunderclap headache. Other causes include reversible cerebral vasoconstriction syndrome (RCVS) or pituitary apoplexy. Still, every thunderclap headache needs urgent imaging-CT first, then MRI if the CT is normal. Never ignore it.
Can a migraine have neurological symptoms like weakness?
Yes, but only in migraines with aura-and even then, the symptoms are different. Migraine aura develops slowly over 5 to 20 minutes and usually resolves within an hour. Stroke symptoms come on suddenly, worsen quickly, and don’t fade. If you have weakness or speech trouble that lasts longer than an hour, or if it’s your first time experiencing it, treat it as a stroke until proven otherwise.
What if I’m over 50 and have a headache but no other symptoms?
New-onset headaches after 50 need evaluation, even without other symptoms. While not every one is serious, the risk of giant cell arteritis or brain tumor rises sharply. A simple blood test and physical exam can rule out the most dangerous causes. If the headache is different from any you’ve had before, get it checked. Don’t assume it’s just aging.
Do I need an MRI or CT scan for a red flag headache?
CT is the first test-it’s fast and good at spotting bleeding. But if the CT is normal and suspicion remains (like with thunderclap headache), an MRI is needed within 4 hours. MRI is better at detecting small tumors, early inflammation, and subtle pressure changes. For papilledema or progressive headaches, MRI is preferred because it’s 22% more sensitive than CT.
Can vaccines cause dangerous headaches?
Most vaccine-related headaches are mild and short-lived. But the International Headache Society now lists new-onset headache with neurological symptoms (like weakness, vision loss, or confusion) after vaccination as a red flag. The CDC has recorded 0.8 cases per 100,000 mRNA doses with neurological involvement. These are extremely rare-but if they happen, they require immediate evaluation.
How do I know if my headache is serious enough to go to the ER?
Use this quick checklist: Did it start suddenly and peak in under a minute? Do you have weakness, speech trouble, vision loss, fever, neck stiffness, confusion, or vomiting after a head injury? Are you over 50 with a new headache? Are you immunocompromised? If you answered yes to any of these, go to the ER now. Don’t wait. Don’t call your doctor first. Emergency care saves lives.
Can stress or dehydration cause a headache that feels like a red flag?
Stress and dehydration can cause bad headaches, but they don’t cause sudden neurological symptoms like weakness, slurred speech, or vision loss. If your headache is accompanied by those signs, it’s not stress. It’s not dehydration. It’s something serious. Don’t confuse the two. When in doubt, get checked.
