Embolism-Anemia Risk Assessment Tool
Enter your information and click "Assess Your Risk" to see your personalized risk evaluation.
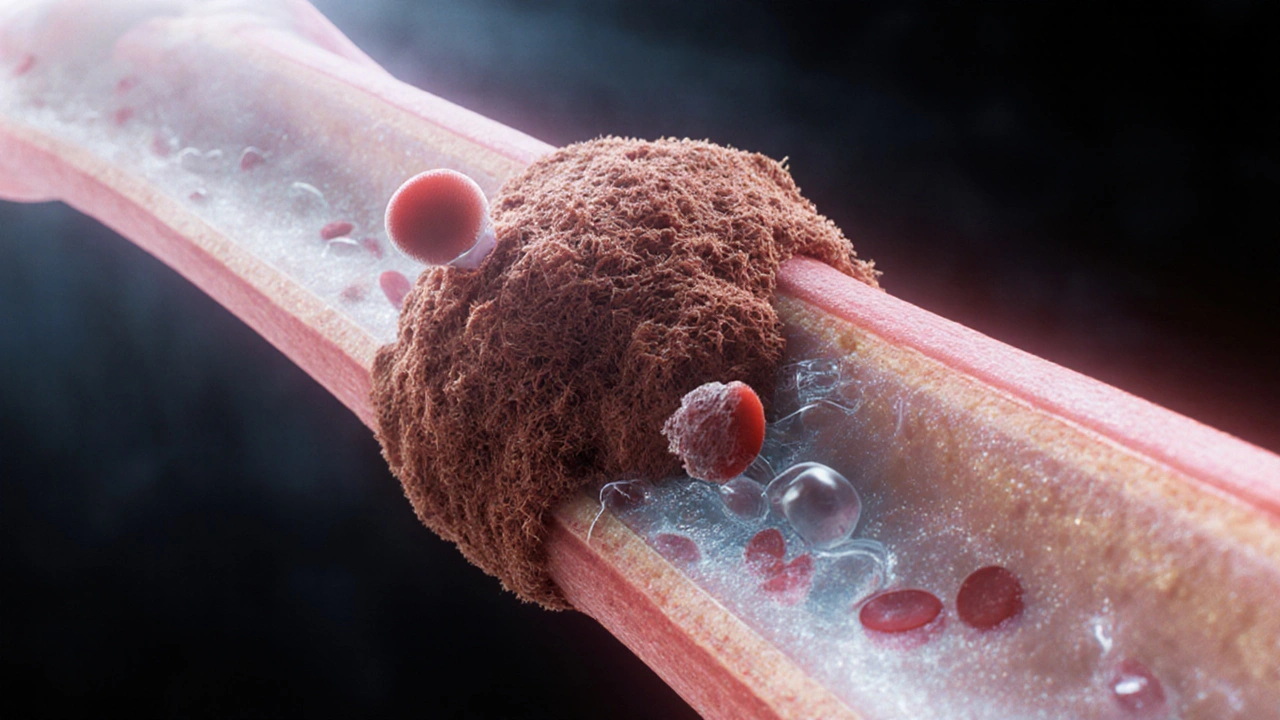
When a blood clot travels to the lungs or brain, doctors call it a Embolism a blockage of a blood vessel caused by a clot, fat, air, or other material that moves from its original site. At the same time, many patients struggle with Anemia a condition where the blood lacks enough healthy red blood cells or hemoglobin to carry adequate oxygen. On the surface they look like unrelated problems, but a growing body of clinical evidence shows that they can influence each other in surprising ways.
Key Takeaways
- Embolism and anemia share physiological pathways, especially through oxygen delivery and blood viscosity.
- Severe anemia can increase the risk of clot formation, while large emboli can worsen anemia by damaging red blood cells.
- Common triggers include chronic inflammation, malignancy, and certain medications.
- Recognizing overlapping symptoms-shortness of breath, fatigue, sudden chest pain-helps catch both conditions early.
- Management often combines anticoagulant therapy with iron supplementation or blood transfusion, tailored to the individual’s risk profile.
What Exactly Is an Embolism?
An embolism starts as a Blood clot a gel‑like mass of fibrin, platelets, and trapped cells that forms to stop bleeding in a vein or artery. When part of that clot breaks off, it becomes an Embolus the traveling fragment that can lodge in a smaller vessel downstream. The most feared types are:
- Pulmonary embolism a clot that blocks one of the lung’s arteries, causing sudden shortness of breath and chest pain.
- Deep vein thrombosis (DVT) a clot that forms in the deep veins of the legs and can later break off, becoming a pulmonary embolism.
- Arterial embolism a clot that travels to brain or limb arteries, potentially causing stroke or limb ischemia.
Understanding Anemia
Anemia isn’t a single disease; it’s a symptom group with multiple causes. The most common form in adults is Iron‑deficiency anemia low hemoglobin caused by insufficient dietary iron, chronic blood loss, or poor absorption. Other types include:
- Vitamin B12 deficiency impairs red blood cell maturation, leading to megaloblastic anemia.
- Sickle‑cell disease a genetic disorder where abnormal hemoglobin causes red cells to deform and break down.
Regardless of the cause, the core problem is reduced Hemoglobin the protein inside red blood cells that binds oxygen and thus lower oxygen delivery to tissues.
How the Two Conditions Interact
At first glance, a clot blocking blood flow and a lack of red cells seem opposite-one adds material, the other takes away. The link lies in the body’s response to low oxygen (Hypoxia insufficient oxygen at the cellular level).
- Increased Blood Viscosity: Severe anemia reduces the number of red cells, making plasma a larger proportion of blood. Paradoxically, the blood can become more viscous in certain inflammatory states, promoting clot formation.
- Platelet Activation: Chronic hypoxia stimulates the bone marrow to release more platelets, raising the risk of thrombosis the formation of clots inside blood vessels.
- Endothelial Damage: Low oxygen damages the lining of vessels (the endothelium). A damaged endothelium loses its natural anti‑clotting properties, making emboli more likely.
- Secondary Bleeding: Large emboli can cause tissue necrosis that leads to internal bleeding. The resulting blood loss may worsen anemia, creating a vicious cycle.
Clinical studies from 2022‑2024 show that patients with chronic anemia have a 1.5‑fold higher incidence of DVT and pulmonary embolism, especially when combined with chronic inflammatory diseases like rheumatoid arthritis.
Risk Factors That Push Both Together
Some scenarios stack the odds for both conditions:
- Cancer: Tumors release pro‑coagulant factors and can cause anemia through marrow infiltration or chemotherapy.
- Autoimmune Disorders: Conditions such as lupus trigger both clotting (antiphospholipid syndrome) and anemia (autoimmune hemolysis).
- Major Surgery: Blood loss leads to anemia, while immobility raises DVT risk.
- Hormone Therapy: Estrogen‑based treatments increase clotting risk; some formulations also interfere with iron metabolism.
- Obesity: Higher body mass raises venous pressure (promoting DVT) and can cause chronic low‑grade inflammation that aggravates anemia.
Recognizing Overlapping Symptoms
Because both conditions affect oxygen transport, the symptoms often look alike. Key warning signs that merit a medical check include:
- Sudden, unexplained shortness of breath-especially after a period of inactivity.
- Sharp chest or back pain that worsens with deep breathing.
- Rapid heart rate (tachycardia) at rest.
- Unusual fatigue that doesn’t improve with sleep.
- Pale skin or nail beds coupled with swelling in the legs.
If you notice a combination of these cues, especially after surgery or a prolonged flight, call your healthcare provider promptly.
Diagnostic Tools
Doctors use a mix of blood tests and imaging to untangle the two problems.
| Test | What It Detects | Typical Findings in Embolism | Typical Findings in Anemia |
|---|---|---|---|
| D‑dimer | Fibrin degradation product | Elevated (suggests clot breakdown) | Usually normal |
| CT Pulmonary Angiography | Imaging of lung arteries | Filling defects indicating a clot | Not useful |
| Complete Blood Count (CBC) | Red cell count, hemoglobin, hematocrit | Often normal unless chronic hypoxia | Low hemoglobin, low hematocrit |
| Iron Studies (Ferritin, Transferrin Saturation) | Body iron stores | Usually normal | Low ferritin, low saturation |
Treatment Strategies That Address Both
Modern guidelines recommend a two‑pronged approach when embolism and anemia coexist.
- Anticoagulation: Low‑molecular‑weight heparin or direct oral anticoagulants (DOACs) prevent further clot propagation. Dose adjustments may be needed if hemoglobin is very low to avoid bleeding.
- Iron Repletion: Oral ferrous sulfate is first‑line for iron‑deficiency anemia. In severe cases, intravenous iron or red‑cell transfusion is used to raise hemoglobin quickly, stabilizing oxygen delivery.
- Address Underlying Causes: Treating inflammation (e.g., with biologics for rheumatoid arthritis) reduces both clotting tendency and anemia of chronic disease.
- Lifestyle Modifications: Regular movement, adequate hydration, and a balanced diet rich in iron (red meat, beans, leafy greens) lower risk on both fronts.
Physicians monitor for complications-like bleeding from anticoagulants or iron overload from excess supplementation-so regular follow‑up labs are essential.
Prevention Tips You Can Use Today
- Stay active: A 10‑minute walk every hour during long flights or desk work keeps blood flowing.
- Hydrate: Dehydration thickens plasma, making clots more likely.
- Eat iron‑rich foods: Pair plant‑based iron with vitamin C to improve absorption.
- Know your meds: Some birth‑control pills and hormone therapies increase clot risk-talk to your doctor about alternatives if you have anemia.
- Screen regularly: If you have chronic conditions (cancer, lupus), get routine CBC and D‑dimer checks as part of your care plan.
When to Call a Doctor
If you experience any of the following, seek care right away:
- Sudden intense chest pain or pressure.
- Shortness of breath that worsens quickly.
- Swelling, redness, or warmth in one leg.
- Fainting or rapid heartbeat accompanied by pale skin.
These could signal a life‑threatening embolism, especially when combined with anemia‑related fatigue.
Frequently Asked Questions
Can anemia cause a blood clot?
Yes. Severe anemia can trigger platelet activation and increase blood viscosity in certain inflammatory states, both of which raise the chance of clot formation.
What symptoms overlap between embolism and anemia?
Both can cause shortness of breath, rapid heart rate, and general fatigue. The key difference is that embolism often adds chest or back pain and leg swelling.
Is it safe to take blood thinners if I have low hemoglobin?
Doctors can prescribe lower doses or switch to a DOAC with a safer bleeding profile, but they will monitor your blood counts closely.
How quickly can iron supplements improve anemia‑related clot risk?
Oral iron typically raises hemoglobin by 1‑2 g/dL over 4‑6 weeks. Intravenous iron can boost levels within days, which may reduce clot‑promoting inflammation faster.
Should I get screened for clotting disorders if I have chronic anemia?
If you have additional risk factors-family history of thrombosis, recent surgery, or an autoimmune disease-your doctor may order a thrombophilia panel alongside anemia work‑up.
Understanding the tie between embolism and anemia helps you spot warning signs early, make smarter lifestyle choices, and partner effectively with your healthcare team. By watching blood health from both the clot and the red‑cell side, you reduce the odds of a dangerous cascade and stay healthier in the long run.