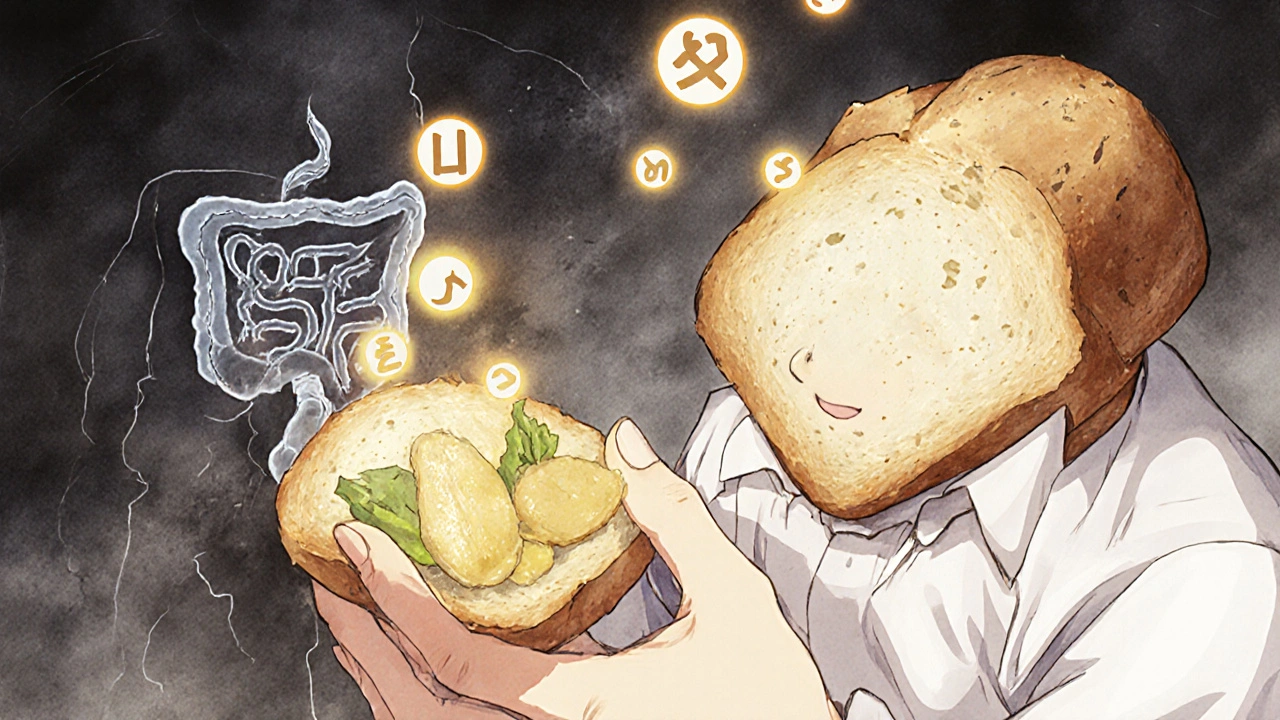
Celiac disease isn’t a food allergy. It’s not a digestive quirk. It’s a full-blown autoimmune attack on your own small intestine-triggered by something as common as bread, pasta, or even soy sauce. Every time someone with celiac eats gluten, their immune system doesn’t just react-it wages war on the very lining of their gut. This isn’t a mild upset. It’s destruction. Villi, the tiny finger-like projections that absorb nutrients, get flattened. Nutrients vanish. Fatigue sets in. Diarrhea, bloating, joint pain, and even depression can follow. And the only treatment? A lifelong, total, 24/7 elimination of gluten. No exceptions. No half-measures.
How Gluten Turns Into an Enemy Inside Your Body
Gluten isn’t naturally toxic. It’s a protein in wheat, barley, and rye. But for people with celiac disease, it becomes a trigger for chaos. The process starts in the gut. When gluten is digested, it doesn’t break down completely. A stubborn fragment called the 33-mer gliadin survives. Normally, your gut lining keeps things like this out. But in celiac disease, a protein called zonulin opens gaps between gut cells-letting gluten fragments slip through.
Once inside, tissue transglutaminase 2 (TG2), an enzyme in your intestinal wall, chemically alters the gluten piece. It changes glutamine into glutamate. This tiny tweak makes the gluten fragment stick like glue to special immune markers called HLA-DQ2 or HLA-DQ8. These are genetic flags you’re born with. About 90% of celiac patients carry HLA-DQ2. Most of the rest have HLA-DQ8. If you don’t have one of these, you won’t develop celiac disease-even if you eat gluten every day.
Now the real damage begins. Immune cells spot this altered gluten and sound the alarm. CD4+ T cells activate, releasing interferon-gamma and interleukin-21. These chemicals turn the gut lining into a war zone. Inflammation spikes. Villi shrink. The surface area for absorbing food drops by up to 70%. That’s why people with untreated celiac often have iron deficiency, low vitamin D, and unexplained weight loss.
A 2024 study from McMaster University changed everything. Scientists found the gut lining itself isn’t just a victim-it’s an active instigator. Cells in the epithelium can actually express the same immune markers (MHC class II) that usually belong to immune cells. This means your gut cells can directly kickstart the attack. It’s not just the immune system misfiring. Your gut is helping it happen.
Celiac vs. Gluten Sensitivity: Why the Difference Matters
Many people think if you feel better off gluten, you have celiac. That’s not true. Non-celiac gluten sensitivity (NCGS) is real-but it’s a different beast. While celiac affects about 1 in 100 people globally, NCGS may affect up to 13% in some populations. But here’s the key difference: NCGS doesn’t cause intestinal damage. No villous atrophy. No autoimmune markers.
Celiac disease has clear, measurable signs. Blood tests show high levels of anti-tTG antibodies-over 98% accurate when you’re still eating gluten. A biopsy of the small intestine confirms it: Marsh stage 3, with flattened villi. NCGS has no such test. No antibodies. No visible damage. Diagnosis is a process of elimination.
And the dietary rules? Celiac demands absolute silence on gluten. Even 20 parts per million (ppm)-the legal limit for “gluten-free” labeling-is too much. One crumb of regular bread can reignite inflammation. NCGS patients may tolerate small amounts. Some can handle a bite of pasta without symptoms. That’s why misdiagnosis is dangerous. Treating NCGS like celiac is unnecessary. Treating celiac like NCGS is life-threatening.
The Only Treatment: A Gluten-Free Diet That’s Not Optional
There’s no pill. No cure. No vaccine. The only proven treatment is a strict, lifelong gluten-free diet. That means no wheat, barley, rye, or any derivatives-malt, brewer’s yeast, hydrolyzed wheat protein, modified food starch unless labeled gluten-free. Even oats are risky unless certified gluten-free, because they’re often cross-contaminated in fields or factories.
Getting started means a full pantry reset. The average cost? $350 to $500. You’ll need new toasters, cutting boards, and utensils. Even a single crumb from a shared toaster can contaminate your gluten-free bread. Studies show using a dedicated gluten-free toaster reduces cross-contamination risk by 85%.
Learn to read labels like a detective. “Natural flavors,” “spices,” “starch,” “dextrin”-any of these could hide gluten. Medications are a hidden trap. Only 37% of prescription drugs list gluten content. A simple pill for acid reflux might contain wheat starch. Always check with your pharmacist.
Gluten-free products cost, on average, 242% more than regular ones. A loaf of gluten-free bread can be $6. A regular one? $2.50. That’s not just inconvenient-it’s a financial burden. Many insurance plans don’t cover these costs. Only 12% of U.S. health plans do.
But the payoff? Huge. In a 2023 survey of over 15,000 celiac patients, 89% saw major improvement within six months of going gluten-free. Fatigue lifted. Digestion returned. Skin rashes faded. One patient, after five years on the diet, had a follow-up endoscopy showing complete mucosal healing. That’s the goal: not just feeling better, but letting your gut repair itself.
Real Challenges: Hidden Gluten, Social Isolation, and Delayed Diagnosis
Most people wait years to get diagnosed. The average? 6.7 years. Why? Symptoms vary wildly. Some have severe diarrhea. Others have anemia, osteoporosis, or infertility. Many are told they have IBS. One Reddit user waited seven years and saw four gastroenterologists before getting a biopsy that confirmed celiac disease.
Even after diagnosis, 42% still have symptoms. Why? Cross-contamination. Dining out is a minefield. A shared fryer fries gluten-free fries in the same oil as breaded chicken. A server wipes a knife with a towel that touched a bagel. Sixty-seven percent of patients report accidental exposure at restaurants.
And the emotional toll? Fifty-eight percent say their quality of life suffers. Birthday parties, work lunches, family dinners-every meal becomes a risk assessment. Young adults avoid social events. Parents stress over school lunches. The isolation is real.
Tools help. Apps like Find Me Gluten Free (rated 4.7 stars from 185,000 reviews) list safe restaurants. Carrying emergency snacks (92% of experienced patients do this) prevents panic when options vanish. Keeping a food journal helps spot patterns-what triggered a flare-up? Was it a new brand of soy sauce? A hotel breakfast?

What’s Next? The Future Beyond the Diet
While the gluten-free diet works, it’s brutal. Researchers are racing to find alternatives. Three therapies are in advanced trials.
Nexvax2 is a vaccine-like treatment using gluten peptides to retrain the immune system. In Phase 2 trials, it cut symptom severity by 42%. Latiglutenase is an enzyme pill that breaks down gluten before it triggers a reaction. In trials, it improved symptoms by 37%. TAK-101 uses nanoparticles to teach the immune system to tolerate gluten. One study showed a 63% reduction in intestinal damage.
Other breakthroughs? Scientists are developing handheld devices that can detect gluten at 5 ppm-far more sensitive than current tests. They’re also studying the gut microbiome. People with celiac have different gut bacteria than healthy people. Could fixing that help? Maybe.
But here’s the truth: even if these therapies work, they won’t replace the gluten-free diet anytime soon. The best hope is combination therapy-something that reduces the damage from accidental exposure, so you don’t have to live in fear of every crumb.
Final Reality Check
Celiac disease is not a trend. It’s not a fad. It’s a lifelong autoimmune condition with serious consequences if ignored. The gluten-free diet isn’t a lifestyle choice-it’s medical necessity. You can’t cheat it. You can’t wish it away. But you can master it.
Know your triggers. Test your environment. Use apps. Talk to your doctor. Join a support group. You’re not alone. Over 1 in 100 people live with this. And with every year, more people get diagnosed, more products become available, and more restaurants learn to cook safely.
Healing takes time. But it happens. And for the first time in your life, you might feel like yourself again.
Can you outgrow celiac disease?
No. Celiac disease is a lifelong genetic condition. Once diagnosed, you must avoid gluten for life. Even if symptoms disappear after going gluten-free, the immune system still reacts to gluten. Eating it again will cause damage, even if you feel fine.
Is a gluten-free diet healthy if you don’t have celiac?
Not necessarily. Many gluten-free products are lower in fiber, iron, and B vitamins because they’re made with refined rice or potato starch instead of whole wheat. Unless you’re avoiding gluten for medical reasons, cutting it out doesn’t improve health-and can lead to nutrient gaps. Don’t go gluten-free without a diagnosis.
Can you test for celiac disease without eating gluten?
No. Blood tests for tTG antibodies and biopsies require active gluten consumption to show results. If you’ve already gone gluten-free, you’ll need to reintroduce gluten for 6-8 weeks under medical supervision before testing. This is called a gluten challenge.
What foods are naturally gluten-free?
Fruits, vegetables, meat, fish, eggs, dairy, legumes, nuts, seeds, rice, quinoa, corn, buckwheat, millet, and certified gluten-free oats are all naturally gluten-free. Always check labels on processed versions-like flavored rice or canned soups-because additives often contain hidden gluten.
Why do some people with celiac still have symptoms on a gluten-free diet?
Up to 30% of patients continue to have symptoms despite following the diet. This can be due to accidental gluten exposure (cross-contamination), other conditions like IBS or lactose intolerance, or incomplete healing. In rare cases, it may indicate refractory celiac disease, where the immune system keeps attacking even without gluten. A follow-up biopsy and nutritional assessment are needed.
Are gluten-free medications safe?
Not always. Only 37% of prescription drugs list gluten content. Fillers like starch, dextrin, or maltodextrin can contain gluten. Always ask your pharmacist to check the inactive ingredients. Some pharmacies offer gluten-free medication lists. Never assume a pill is safe just because it’s labeled “natural” or “vegetarian.”
Can celiac disease be diagnosed with a blood test alone?
No. Blood tests (like tTG-IgA) are highly accurate-over 98% sensitive-but they’re only reliable if you’re still eating gluten. A positive blood test must be confirmed with a small intestine biopsy. That’s the gold standard. Genetic testing (for HLA-DQ2/DQ8) can rule out celiac, but not confirm it.
How long does it take for the gut to heal after going gluten-free?
Children often heal within 3-6 months. Adults may take 1-2 years, sometimes longer. Healing depends on age, how long the disease went untreated, and how strictly the diet is followed. Follow-up endoscopies are the only way to confirm mucosal recovery. Don’t assume you’re healed just because you feel better.
