Why Grapefruit Juice Can Be Dangerous With Your Medications
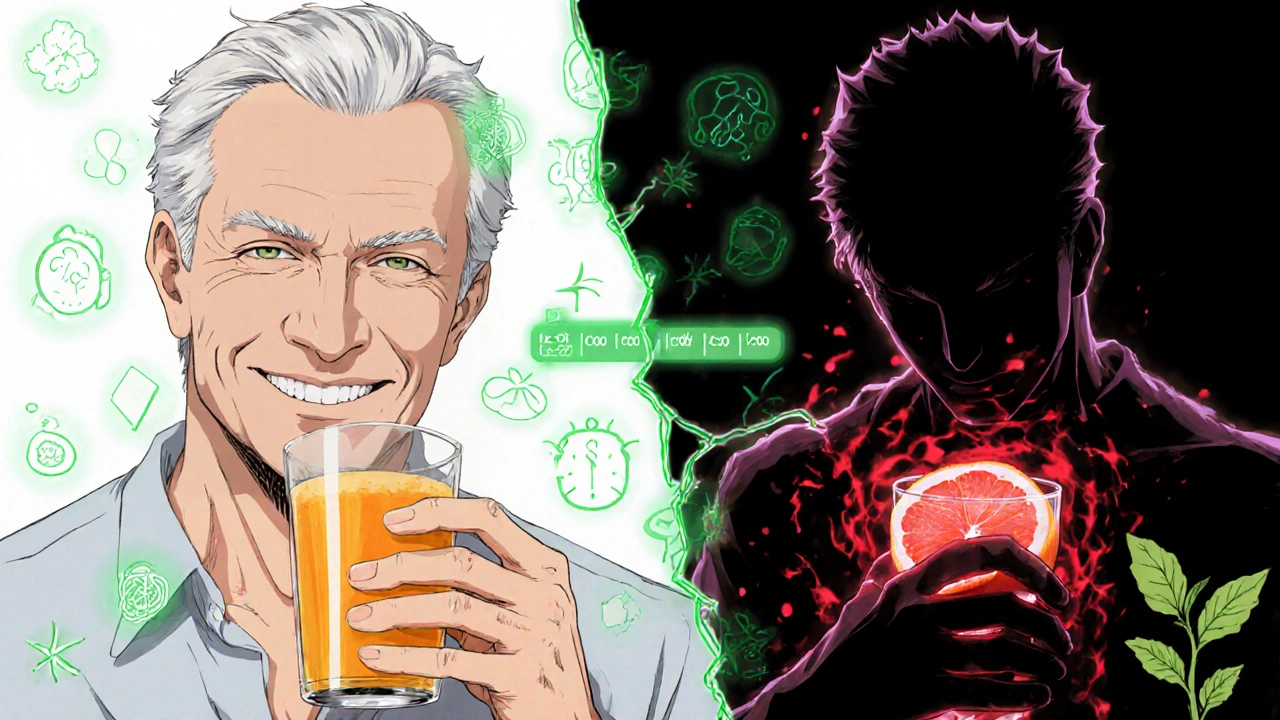
You might think a glass of grapefruit juice is just a healthy start to the day-vitamin C, antioxidants, refreshing taste. But if you’re taking certain medications, that juice could be hiding a serious risk. It’s not about allergies or sugar. It’s about something deeper: your body’s ability to process your drugs properly.
Back in 1989, researchers in Canada noticed something strange. People taking the blood pressure drug felodipine had way higher levels of the drug in their blood after drinking grapefruit juice. It wasn’t a coincidence. They found that grapefruit juice was blocking a key enzyme in the gut called CYP3A4. This enzyme normally breaks down about half of all oral medications before they enter your bloodstream. When it’s shut down, too much drug gets through-and stays around too long.
The FDA now says this isn’t just a theory. It’s a documented danger. More than 85 prescription drugs have confirmed interactions with grapefruit juice. Of those, 43 can cause life-threatening reactions like heart rhythm problems, kidney failure, or muscle breakdown. And the worst part? You don’t need to drink a whole pitcher. One 200-milliliter glass-about a cup-is enough to start the effect.
How Grapefruit Juice Disrupts Your Medications
The culprit isn’t sugar or acid. It’s a group of natural chemicals called furanocoumarins-mainly bergamottin and 6’,7’-dihydroxybergamottin. These compounds don’t just slow down the CYP3A4 enzyme. They destroy it. And once that enzyme is gone, your body can’t make more for 24 to 72 hours.
That means even if you take your pill at 8 a.m. and drink grapefruit juice at 6 p.m., the damage is already done. The enzyme in your gut is already shut off. The next morning’s dose? It’s going straight into your bloodstream with no filter.
This isn’t a short-term glitch. It’s a long-lasting change. Studies show that a single glass of fresh grapefruit juice can reduce intestinal CYP3A4 activity by 47% within four hours. The effect peaks at 24 hours and can last up to three days. That’s why experts say you can’t just avoid grapefruit juice around your pill time. You have to avoid it for the entire time you’re on the medication.
Not all grapefruit is the same. White grapefruit has more furanocoumarins than red. Fresh-squeezed juice is stronger than pasteurized. Even eating the fruit whole can cause the same problem. And it’s not just juice-grapefruit extract, supplements, and even some cosmetics with grapefruit oil can trigger reactions.
Medications That Can’t Mix With Grapefruit Juice
Some drugs are far more dangerous when mixed with grapefruit than others. Here are the big ones:
- Statins (cholesterol drugs): Simvastatin (Zocor) is the most risky. One cup of grapefruit juice can triple your blood levels, raising your chance of rhabdomyolysis-a condition where muscle tissue breaks down and can cause kidney failure. Atorvastatin (Lipitor) has a smaller but still real risk. Pravastatin and rosuvastatin? Safe. No interaction.
- Calcium channel blockers (blood pressure drugs): Felodipine (Plendil) sees a five-fold increase in blood levels. Nifedipine (Procardia) jumps by 3.3 times. Amlodipine (Norvasc)? Minimal effect. Your doctor may switch you if you love citrus.
- Immunosuppressants: Cyclosporine (Neoral), used after organ transplants, can spike by 50-60% with grapefruit. That raises the risk of kidney damage. Tacrolimus is a safer alternative.
- Antiarrhythmics: Amiodarone (Cordarone) can lead to dangerous heart rhythms when levels rise. Even a small increase can be risky.
- Some psychiatric drugs: Certain antidepressants and sedatives interact, but not all. Trazodone and zolpidem show little to no interaction. Always check.
The FDA requires drugmakers to list grapefruit warnings on labels for 76% of affected medications. But many patients never see it. If your prescription doesn’t say anything, don’t assume it’s safe. Ask your pharmacist.

What About Other Citrus Fruits?
Not all citrus is the same. Seville oranges (used in traditional marmalade) and pomelos contain the same furanocoumarins as grapefruit. So if you’re on a high-risk drug, avoid those too.
But sweet oranges-like navel or Valencia-? Safe. Lemons? Safe. Limes? Mostly safe, though some varieties may have trace amounts. The European Medicines Agency confirms that regular orange juice and lemon juice don’t cause these interactions.
So you don’t have to give up citrus entirely. Just know the difference. If you’re unsure, check the label or ask your pharmacist. A quick look at the fruit’s name can save you from a hospital visit.
Who’s Most at Risk?
Older adults are the most vulnerable group. People over 65 make up 40% of grapefruit juice drinkers in the U.S., according to USDA data. They’re also more likely to be on multiple medications-three to five on average. That increases the chance of hitting one of those 85 risky drugs.
And here’s the catch: you can’t predict who will have a severe reaction. One study found that when people drank grapefruit juice with felodipine, drug levels ranged from zero to eight times higher than normal. Why? Because people naturally have different amounts of CYP3A4 in their guts. Some have almost none. Others have a lot. You won’t know which you are.
That’s why experts like Dr. David Bailey-who discovered the interaction-say the only safe rule is: avoid grapefruit entirely if you’re on a high-risk drug. No exceptions. No "just a little." One glass can be the difference between a normal day and an emergency room visit.
What Should You Do?
Here’s what works in real life:
- Know your meds. Make a list of every pill, patch, or supplement you take. Include over-the-counter drugs like antihistamines (fexofenadine/Allegra) and sleep aids.
- Ask your pharmacist. When you pick up a new prescription, ask: "Does this interact with grapefruit?" Pharmacists are trained to catch this. One 2021 study found 89% of community pharmacists screen for it.
- Check the label. Look for "avoid grapefruit" or "do not consume grapefruit products" on the patient information sheet.
- Consider alternatives. If you love grapefruit and take simvastatin, ask your doctor about switching to pravastatin or rosuvastatin. No interaction. Same benefit.
- Be consistent. If you’re told to avoid it, avoid it for the entire time you’re on the drug. Not just when you take the pill. Not just on weekends. All the time.
It’s not about being paranoid. It’s about being informed. Medications are powerful. Grapefruit juice is powerful. Together, they can be deadly.
What’s Changing? New Research and Future Solutions
Scientists are working on solutions. In October 2023, the USDA announced that CRISPR-edited grapefruit with 90% less furanocoumarin had passed early safety tests. If approved, these "safe grapefruits" could hit the market in the next few years.
Meanwhile, drugmakers are required by the FDA to test all new oral drugs for grapefruit interactions. The European Medicines Agency now demands the same. This means fewer risky drugs will enter the market in the future.
But until then, the rule stays simple: if your drug interacts with grapefruit, don’t drink it. Don’t gamble. Don’t assume you’re fine because you’ve had it before. Your body changes. Your meds change. The risk doesn’t go away.
There’s no shortcut. No magic workaround. Just one clear choice: protect your health by keeping grapefruit juice away from your pills.
Can I drink grapefruit juice if I take my medication at a different time of day?
No. Grapefruit juice permanently disables the CYP3A4 enzyme in your gut for up to 72 hours. Even if you take your pill 12 hours after drinking juice, the enzyme is still blocked. The interaction doesn’t depend on timing-it depends on whether the enzyme is active. Avoid grapefruit entirely while on the medication.
Is grapefruit juice dangerous with over-the-counter drugs?
Yes. Some OTC medications can interact. Fexofenadine (Allegra), a common allergy pill, has reduced effectiveness with grapefruit juice. Other antihistamines and sleep aids may also be affected. Always check the label or ask your pharmacist before combining any drug with grapefruit.
Are there any safe citrus fruits I can drink instead?
Yes. Sweet oranges (navel, Valencia), lemons, and limes do not contain furanocoumarins and are safe to consume with most medications. Seville oranges and pomelos are not safe-they act like grapefruit. Always check the specific fruit type, not just "citrus."
What should I do if I accidentally drank grapefruit juice with my medication?
If you’ve taken a high-risk medication like simvastatin, felodipine, or cyclosporine and drank grapefruit juice, watch for symptoms like unexplained muscle pain, weakness, dark urine, dizziness, or irregular heartbeat. Call your doctor or pharmacist immediately. Don’t wait. The interaction can be life-threatening, even if you feel fine now.
Can I switch to a different statin to avoid this problem?
Yes. If you’re on simvastatin and want to keep drinking grapefruit juice, talk to your doctor about switching to pravastatin or rosuvastatin. These statins don’t rely on CYP3A4 for metabolism and have no known interaction with grapefruit. Many patients make this switch safely with no loss of cholesterol control.
