Heartburn hits hard - that burning feeling in your chest, the sour taste in your throat, the sleepless nights. If you’ve ever reached for a bottle of Tums, Pepcid, or Prilosec without a prescription, you’ve used an OTC heartburn medication. But not all of them work the same way, and not all are meant for the same kind of heartburn. Knowing the difference between antacids, H2 blockers, and PPIs can save you money, prevent side effects, and finally get you real relief.
Antacids: Fast But Short-Lived
Antacids are the OG of heartburn relief. They’ve been around since the 1800s. Think Tums, Rolaids, or Milk of Magnesia. These work by neutralizing stomach acid the moment it hits your esophagus. No waiting. No buildup. Just chemical reaction.
Calcium carbonate (in Tums) can neutralize up to 24 mEq of acid per tablet. Aluminum and magnesium hydroxide in other brands do the same. You chew or swallow, and within 30 to 120 seconds, the burning starts to fade. That’s faster than any other OTC option.
But here’s the catch: it doesn’t last. The relief lasts about 45 minutes on average. If you eat a spicy pizza at 8 p.m. and take Tums at 8:15, you’ll likely be back to square pain by 9:00. That’s why people end up popping five or six tablets in one night. It’s not just habit - it’s physics.
Antacids are perfect for occasional heartburn - say, once a week after a big meal. They’re not meant for daily use. And if you’re taking them more than twice a week, you’re masking a deeper problem. Calcium-based antacids can even cause rebound acid production. About 30% of users find their heartburn comes back worse within a couple hours because the stomach overcompensates.
Also, don’t mix them with other meds. Antacids can block absorption of antibiotics, iron, or thyroid meds. If you’re on anything else, wait at least two hours before or after taking an antacid.
H2 Blockers: Slower, But Longer-Lasting
H2 blockers - like Pepcid AC, Tagamet HB, and Axid AR - work differently. Instead of neutralizing acid, they tell your stomach to make less of it. They block histamine, a chemical that signals your stomach cells to pump out acid.
They take longer to kick in - 60 to 180 minutes. So if you’re already burning, they won’t help right away. But once they do, they last 8 to 12 hours. That makes them ideal for predictable heartburn: you know you’re going to eat pizza on Friday night? Take a Pepcid AC an hour before. You get sleep through the night without waking up to acid.
They’re also better than antacids for nighttime heartburn. Studies show famotidine (the active ingredient in Pepcid) reduces nighttime acid by 75%. That’s higher than omeprazole (Prilosec), which only hits 58%.
But H2 blockers have a major flaw: tolerance. After 2 to 3 weeks of daily use, your body starts to adapt. The acid suppression drops from 60-70% down to maybe 30%. That’s why people say, “It worked great at first, then stopped working.” It’s not your imagination. It’s science.
They’re FDA-approved for use up to 14 days at a time, but they’re not meant to be a long-term fix. And they interact with other drugs. Cimetidine (Tagamet HB) can mess with blood thinners like warfarin and seizure meds like phenytoin. Always check labels or ask a pharmacist.
Best for: People who get heartburn 1 to 2 times a week, especially after meals or at night. Not for daily use beyond two weeks.
PPIs: The Heavy Hitters - Use With Care
Proton pump inhibitors - Prilosec OTC, Nexium 24HR, Prevacid 24HR - are the strongest OTC heartburn drugs you can buy without a prescription. They shut down the acid pumps in your stomach cells completely. That’s why they reduce acid production by 90 to 98%.
But here’s the kicker: they don’t work fast. You need 24 to 72 hours to feel the full effect. If you take one at 7 a.m. on Monday and have heartburn at 11 a.m., you’ll still be in pain. That’s why so many people give up on them too soon. They’re not designed for instant relief.
PPIs are meant for frequent heartburn - two or more days a week. A 2022 JAMA study found PPIs reduced symptoms by 90% over 14 days. H2 blockers? Only 65%. That’s why doctors recommend PPIs when other options fail.
But they come with risks. The FDA has issued multiple warnings about long-term PPI use:
- Increased risk of Clostridium difficile infection (1.7x higher)
- Higher chance of hip fractures (35% increase with daily use over a year)
- Low magnesium levels (FDA warning since 2011)
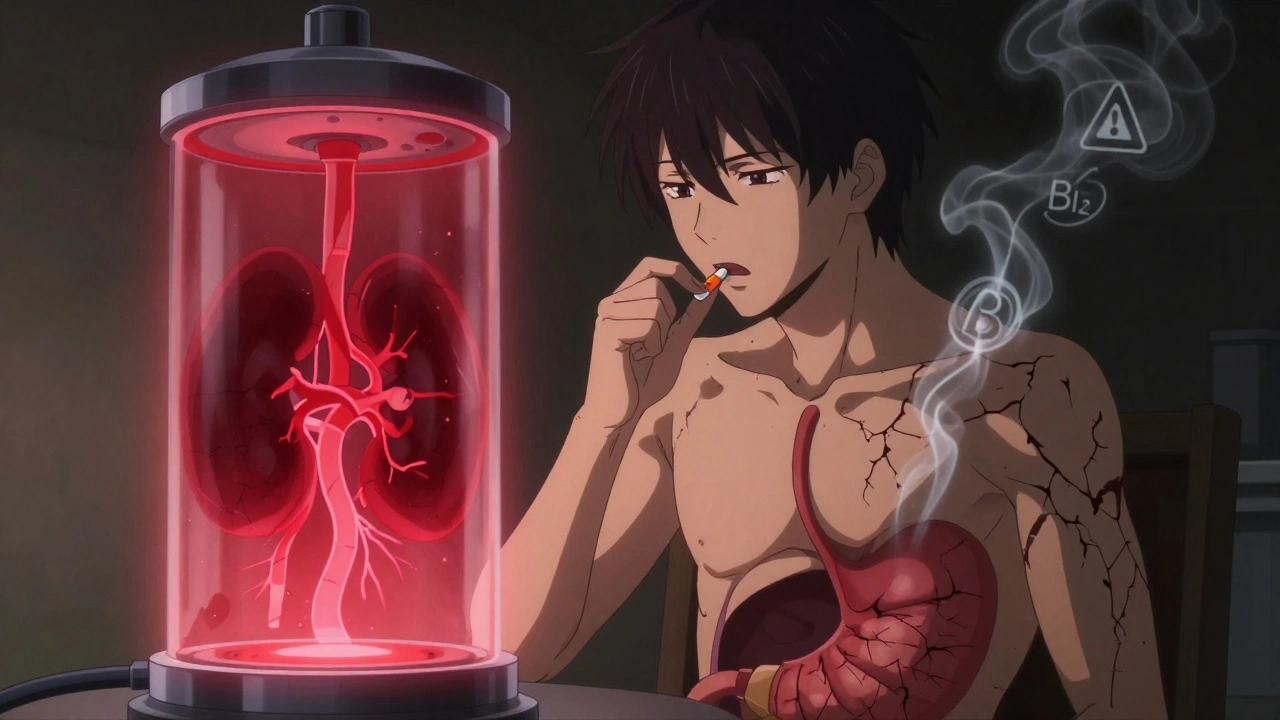
- Lower vitamin B12 absorption (43% of long-term users develop deficiency)
- Possible kidney damage (23% higher risk after one year of daily use, per Johns Hopkins 2023 research)
And the labeling is strict: no more than 14 consecutive days, and only once every four months unless a doctor says otherwise. Yet, a 2023 Consumer Reports survey found 43% of users take PPIs longer than recommended.
Also, timing matters. You must take PPIs 30 to 60 minutes before breakfast. If you take them after eating, or with orange juice (which breaks down the coating), they won’t work. Many users don’t know this. That’s why they say, “It didn’t help.” It’s not the drug - it’s how they took it.
Best for: People with frequent heartburn (≥2 days/week) who’ve tried antacids and H2 blockers without success. Not for occasional use. Not for quick relief.

Which One Should You Choose?
Let’s cut through the noise. Here’s a simple guide based on how often you get heartburn:
- Less than once a week → Antacids (Tums, Rolaids). Chew one when it hits.
- 1 to 2 times a week → H2 blockers (Pepcid AC). Take 30 to 60 minutes before meals you know will trigger it.
- 2 or more days a week → PPIs (Prilosec OTC). Take one daily, 30 minutes before breakfast, for no more than 14 days. Then stop. If it comes back, see a doctor.
And here’s what not to do:
- Don’t use PPIs as a quick fix for a single episode.
- Don’t take H2 blockers every day for months.
- Don’t double up on antacids to make them last longer - you’ll just get side effects like diarrhea (magnesium) or constipation (aluminum).
Many people combine them - and that’s okay, if done right. A 2023 Curist clinical guideline found 68% of frequent heartburn sufferers use antacids for sudden flare-ups while on a PPI. That’s smart. The PPI handles the baseline acid. The antacid handles the spikes.
Real User Experiences
On Amazon, Tums has over 28,000 reviews with a 4.7-star rating. People love the speed. But 63% of negative reviews say, “I had to keep taking more.” That’s the short duration problem.
Pepcid AC has 15,000+ reviews. People who use it for dinner or bedtime say, “It lets me sleep.” But nearly 60% say, “After two weeks, it didn’t work anymore.” That’s tolerance.
Prilosec OTC? 21,000 reviews. 71% say it “saved my life” for daily heartburn. But 67% say, “It took too long to work.” That’s the delayed onset. One Reddit user summed it up: “I take Prilosec every morning. If I get a spike, I chew a Tums. That’s my system.”
Consumer Reports surveyed 1,245 people. 73% started with antacids. 41% moved to H2 blockers within six months. 28% ended up on PPIs. And 37% said their OTC meds weren’t enough - they had to see a doctor.
When to See a Doctor
OTC meds are great for occasional heartburn. But if you need them more than twice a week for more than two weeks, it’s time to talk to a professional. Persistent heartburn can be a sign of GERD, a hiatal hernia, or even Barrett’s esophagus - a condition that raises cancer risk.
Also, if you have any of these symptoms, don’t just pop pills:
- Difficulty swallowing
- Unexplained weight loss
- Vomiting blood or black, tarry stools
- Chest pain that spreads to your arm or jaw
That last one could be a heart attack. Don’t assume it’s heartburn. Get checked.
Bottom Line
OTC heartburn meds are tools, not cures. Antacids are your emergency brake. H2 blockers are your cruise control for predictable triggers. PPIs are your engine shutdown for chronic cases - but they’re not meant to be left on forever.
Use the right one for the right problem. Don’t reach for Prilosec because you ate too much pizza last night. Use Tums. Don’t take Pepcid every day because you’re stressed. Try lifestyle changes first - lose weight, avoid late meals, cut out caffeine. Medication should be the backup, not the plan.
And if you’ve been taking PPIs for more than 14 days without a doctor’s advice - stop. Talk to someone. There are safer, smarter ways to manage your heartburn long-term.
Can I take antacids and PPIs together?
Yes, but not at the same time. Take your PPI 30 to 60 minutes before breakfast. If you get a sudden flare-up later, take an antacid like Tums. Wait at least two hours after the antacid before taking another PPI dose. This avoids interference with absorption.
Why does my heartburn come back after taking Pepcid?
H2 blockers like Pepcid lose effectiveness after 2 to 3 weeks of daily use because your stomach cells adapt. This is called tachyphylaxis. It’s not that the drug stopped working - your body got used to it. Switch to a PPI if symptoms persist, or give your stomach a break for a few days before trying H2 blockers again.
Is it safe to take Prilosec every day?
No. OTC Prilosec is labeled for 14 days only, once every four months. Daily use beyond that increases your risk of kidney damage, low magnesium, vitamin B12 deficiency, and bone fractures. If you need daily acid control for longer, you need a doctor’s evaluation - not an OTC bottle.
Do H2 blockers work better at night than PPIs?
Yes, for some people. Famotidine (Pepcid) reduces nighttime acid by 75%, while omeprazole (Prilosec) only drops it by 58%. If you wake up with heartburn every night, H2 blockers taken before bed may be more effective than PPIs taken in the morning.
Can I take OTC heartburn meds if I’m pregnant?
Antacids like Tums (calcium carbonate) are generally considered safe during pregnancy. H2 blockers like Pepcid are also often approved by OB-GYNs. PPIs are used cautiously and only if needed. Always check with your doctor before taking any medication while pregnant - even OTC ones.
What’s the cheapest option for long-term heartburn?
Generic antacids are the cheapest - Tums can cost as little as $2.99 for 100 tablets. H2 blockers like famotidine (generic Pepcid) cost around $5 for 30 tablets. PPIs like omeprazole are now available as generics for under $5 at pharmacies like Walmart or Costco. Curist’s generic PPIs cost $4.99 per bottle - 80% cheaper than brand names. But remember: cheap doesn’t mean safe for daily long-term use.
Next Steps
If you’ve been self-treating heartburn for months, start here:
- Track your symptoms for one week. When does it happen? After what foods? At what time?
- Try switching to the right OTC med for your frequency - not the one you’ve always used.
- Stop PPIs after 14 days unless directed by a doctor.
- If you’re still having symptoms after 2 weeks of correct OTC use, make an appointment.
Heartburn is common. But it’s not normal to live with it. The right medication, used the right way, can give you your life back - without risking your health.
