Getting sick while traveling is bad enough. But if you're taking prescription meds and don't know how to read your label correctly across time zones, you could end up in a hospital halfway across the world. It happens more often than you think. A traveler in Tokyo gets detained because their ibuprofen bottle doesn't have Japanese kanji. Someone in Prague ends up in the ER after doubling their thyroid dose because they misread "take once daily" as local time. These aren't rare mistakes-they're predictable ones.
What's on Your Prescription Label (And What You Must Check)
Your prescription label isn't just a receipt. It's your medical passport. Before you even pack your bag, check these seven parts:- Patient name - Must match your passport exactly. No nicknames, no initials. If it says "J. Smith" and your passport says "Jennifer Smith," customs may flag it.
- Medication name - Look for both brand and generic names. For example: "Lipitor (atorvastatin)." Many countries only recognize the generic. If your label only says "Xanax," you're at risk in places like Japan or Saudi Arabia.
- Dosage strength - Is it 10mg? 500mg? 20 IU? Don't assume. Some countries measure differently. Liquid meds need concentration (e.g., "5mg/mL").
- Directions for use (the "sig") - This is the most important part. Look for "q24h" (every 24 hours), "q12h" (every 12 hours), or "q8h." Avoid AM/PM. Those are unreliable across time zones.
- Prescriber info - Name, phone, license number. Some countries require this. The U.S. doesn't always include it, but you should ask your pharmacist to add it.
- Pharmacy details - Address and license number. Helps prove legitimacy if questioned.
- Prescription number - For tracking. Useful if you lose your meds or need a refill abroad.
If any of these are missing, call your pharmacy. Most major chains in the U.S. will print an updated label with extra info if you ask. Don’t wait until the airport.
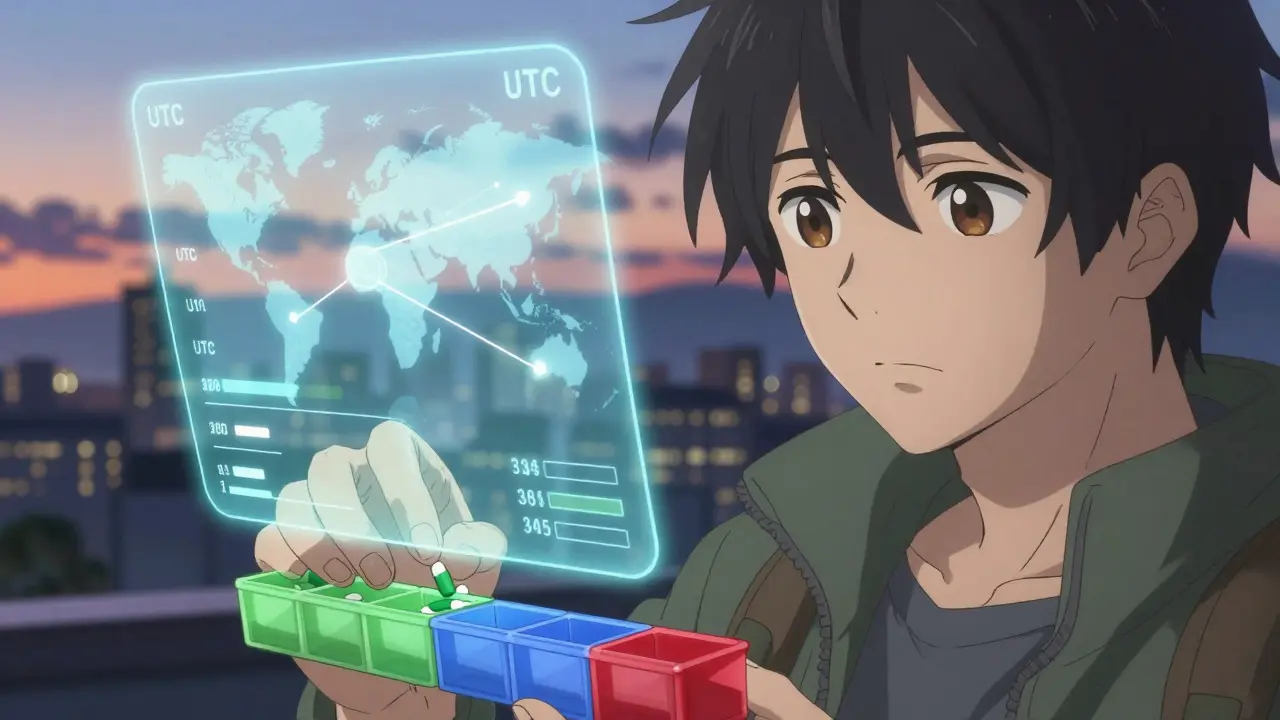
Time Zones Don’t Care About Your Schedule
Your body doesn’t reset when you land. But your meds might need to. The key is Coordinated Universal Time (UTC). Forget local time. Use UTC as your anchor.Example: You take 10mg of levothyroxine every morning at 7:00 AM Eastern Time (UTC-5). You fly to Tokyo (UTC+9). If you keep your home schedule, you’ll take it at 8:00 PM Tokyo time. That’s fine for some meds. But for others-like insulin or blood thinners-it’s dangerous.
Here’s how to handle it:
- For meds with long half-lives (24+ hours) - Like statins, thyroid pills, or antidepressants. Stick to your home schedule for the first 2-3 days. Your body adjusts slowly. Changing too fast can cause side effects.
- For meds with short half-lives (4-12 hours) - Like antibiotics, insulin, or blood thinners. Switch to destination time immediately. If you take a dose every 12 hours, set alarms for 7:00 AM and 7:00 PM local time. Don’t wait for your body to feel "ready."
- For meds with peak effects - Check your label. Does it say "peak effect 2-4 hours after dose"? That tells you how sensitive your body is to timing. Warfarin, for example, has a 40-hour half-life. You can delay a dose by 6-8 hours without risk. But if you’re on a 12-hour antibiotic like amoxicillin? Miss a dose, and the infection can flare up.
Dr. Susan Pisani, a pharmacist at Memorial Sloan Kettering, says: "Knowing the half-life tells you whether you’re in a hurry or can wait. Most travelers don’t check this. They just guess. That’s how mistakes happen."
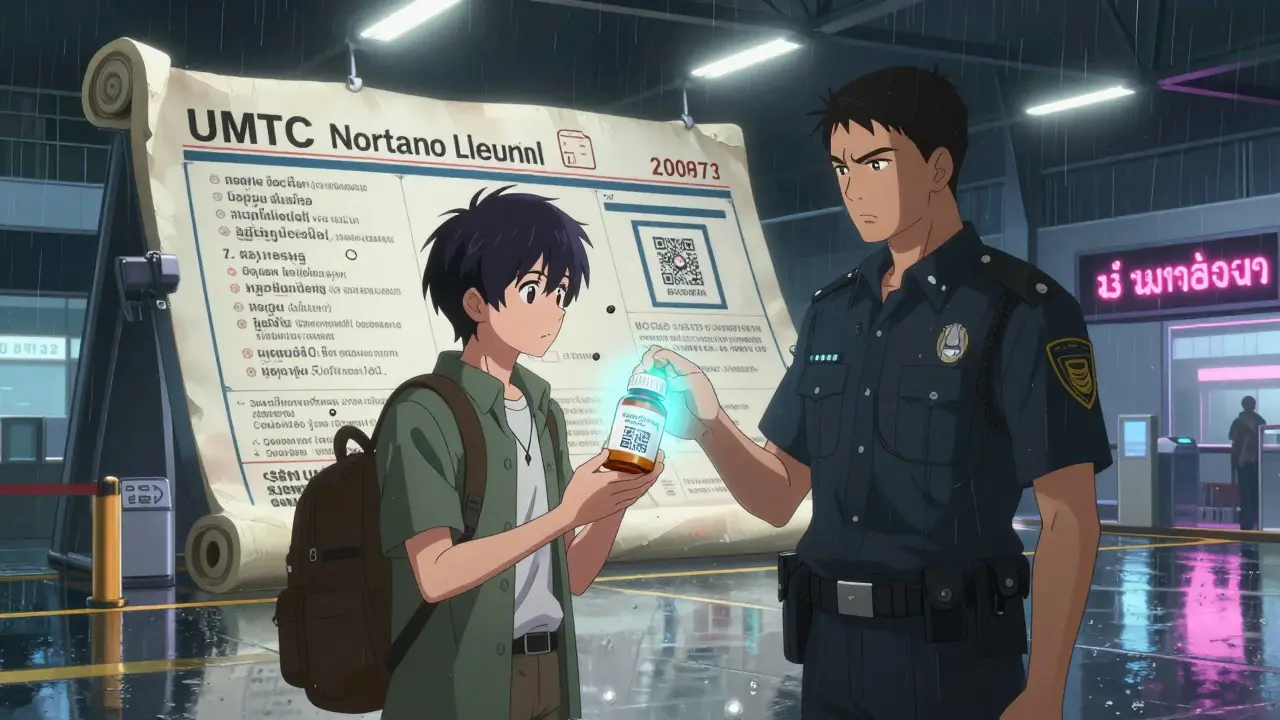
Country Rules Are Not the Same
You can’t assume your U.S. label will fly anywhere. Each country has its own rules:- Japan - Requires kanji for all active ingredients. If your label says "ibuprofen," you’ll be stopped at customs. Ask your pharmacist to add the Japanese name: "イブプロフェン."
- Saudi Arabia - Needs Arabic name of the drug. English-only labels get confiscated. 22% of seized meds at Riyadh Airport in early 2023 were due to missing Arabic text.
- Thailand - Must have both English and Thai. No exceptions.
- European Union - Standardized format, but patient name must be in the local language. If you’re going to Spain, your name needs to be in Spanish (e.g., "Juan Smith").
- Caribbean nations - Many require English and Spanish. Only 37% of U.S. prescriptions meet this. You’ll need to get it fixed before you go.
Check the WHO’s guidelines for your destination. Or use the International Society of Travel Medicine’s checklist-they update it yearly. Don’t rely on Google. Outdated info gets people arrested.
What to Do Before You Leave
Four to six weeks before you go, do this:- Call your pharmacy. Ask them to add: UTC time, generic name, active ingredient concentration (for liquids), and physician license number.
- Request a printed copy of your medication schedule in UTC. Example: "Take 1 tablet at 08:00 UTC (03:00 EST)." Most U.S. pharmacies now do this on request.
- Use the WHO’s free Medication Time Zone Converter app. It auto-adjusts your doses based on your flight path and destination.
- Make a color-coded chart. Green = morning, blue = afternoon, red = night. Tape it to your pill organizer.
- Carry a doctor’s note in English (and local language if possible) explaining why you need the meds. Especially for controlled substances like opioids or stimulants.
One traveler in Reddit’s r/travel community took double doses of levothyroxine because she thought "take on empty stomach" meant "before breakfast"-not realizing breakfast in Prague was 3 hours ahead. She ended up in the hospital. A simple chart could’ve prevented it.
What NOT to Do
- Don’t transfer meds to daily pill organizers unless they’re labeled. TSA says it’s fine, but customs agents don’t care about TSA rules. They see a plastic container with pills and think "illicit." Keep meds in original bottles.
- Don’t rely on airport pharmacists to translate or refill your meds. Many don’t speak English. Some don’t even carry your drug.
- Don’t assume "once daily" means morning. In some cultures, meds are taken at night. Check the label’s instructions-not your assumption.
- Don’t skip your meds for "jet lag". Skipping insulin or anticoagulants can cause blood clots or strokes. Adjust timing, don’t skip.
Tools That Actually Work
- WHO Medication Time Zone Converter - Free app. Download it. Put in your meds, your flight, and it spits out a schedule in UTC and local time.
- International Society of Travel Medicine Checklist - PDF download. Print it. Keep it with your passport.
- GoodRx Travel Medication Tracker - Lets you set alarms in UTC. 89% of users who used it reported zero timing errors.
- Universal Medication Travel Card (UMTC) - Now used by 47 airlines. Get one from your airline’s website. It links your label to country-specific rules.
These aren’t luxuries. They’re insurance. A medical evacuation from a remote location can cost up to $250,000. A 10-minute call to your pharmacy? Free.
What’s Changing in 2025
By the end of 2025, the WHO will require all international prescription labels to include a "travel supplement" section with:- UTC dosing times
- Active ingredient names in 3 languages (English, local language, Spanish)
- A QR code linking to multilingual safety info
Already being tested in Canada, Australia, Singapore, and Dubai. If you’re traveling after 2025, your label will look different. But today? You still have to do the work.
Dr. Robert Steffen, past president of the International Society of Travel Medicine, warns: "Without mandatory global standards, medication errors will keep rising. By 2027, we could see 15,000+ preventable hospitalizations a year just from time zone confusion."
You don’t need to be a doctor to avoid that. Just know what’s on your label-and how to read it.
Can I put my pills in a pill organizer when traveling?
Only if the original bottle is still with you. Customs agents don’t recognize pill organizers. They need to see the original label with your name, drug name, and pharmacy info. Keep your meds in original bottles. Use the organizer as a daily helper, not your main container.
What if my prescription doesn’t have the generic name?
Call your pharmacy. Most will print a new label with both brand and generic names. If they won’t, ask your doctor for a letter that includes the generic name. In countries like Japan or Saudi Arabia, you’ll be turned away without it.
Do I need a doctor’s note for my meds?
For most routine meds, no. But for controlled substances (opioids, ADHD meds, benzodiazepines), yes. Always carry a note on letterhead with your doctor’s signature. Some countries require it by law. Even if they don’t, it saves you hours at customs.
How do I know if a medication has a short or long half-life?
Check the label or ask your pharmacist. Common short half-lives (4-12 hours): antibiotics, insulin, warfarin, ibuprofen. Long half-lives (24+ hours): thyroid meds, statins, antidepressants. If unsure, assume it’s short. Better to adjust than risk missing a dose.
What if I run out of meds while traveling?
Don’t wait. Before you leave, get a 10-15% extra supply. If you do run out, go to a hospital or licensed pharmacy. Don’t buy from street vendors. Many countries have strict rules about foreign prescriptions. Your best bet is to contact your embassy or use the WHO’s global pharmacy locator.
Can I bring liquid meds on a plane?
Yes. Medications are exempt from the 3.4 oz liquid rule. But they must be clearly labeled. For liquids, the label must include concentration (e.g., 5mg/mL). If it doesn’t, you might be asked to discard it. Always carry a doctor’s note for liquids over 100 mL.
Is it safe to adjust my insulin schedule when crossing time zones?
Yes-but only with guidance. Insulin is time-sensitive. Don’t guess. Use the WHO app or talk to your endocrinologist before you go. Most experts recommend switching to destination time immediately for long-acting insulin, but delay short-acting doses by 1-2 hours to avoid low blood sugar. Never skip a dose.
