When you’re taking multiple medications, it’s easy to get lost. One pill in the morning, two at night, a patch that changes weekly, and an over-the-counter supplement you forgot to tell your doctor about. Miss one dose, and you’re not sure if it’s a big deal. Take two by accident, and now you’re worried. This isn’t just confusion-it’s a safety risk. About 280,000 people in the U.S. end up in the hospital every year because of medication errors. But there’s a simple, proven solution: a Medication Action Plan (MAP) made with your care team.
What Is a Medication Action Plan?
A Medication Action Plan isn’t just a list of your pills. It’s a personalized roadmap that tells you exactly what to do, when to do it, and what to watch for. Think of it like a GPS for your meds. Instead of guessing, you have clear steps written out in plain language. It includes your prescription drugs, over-the-counter medicines, vitamins, and even herbal supplements. It also explains why you’re taking each one, what side effects to expect, and what to do if something goes wrong. The plan is created during a Comprehensive Medication Review (CMR), usually done by a pharmacist, but often with input from your doctor and nurse. In Germany, since 2016, anyone on three or more medications gets a standardized version by law. In the U.S., Medicare Part D has required these plans since 2006 for people taking eight or more chronic medications and spending over $4,430 a year on them. But even if you don’t qualify for Medicare, many private insurers now offer them too.Why a Medication Action Plan Works
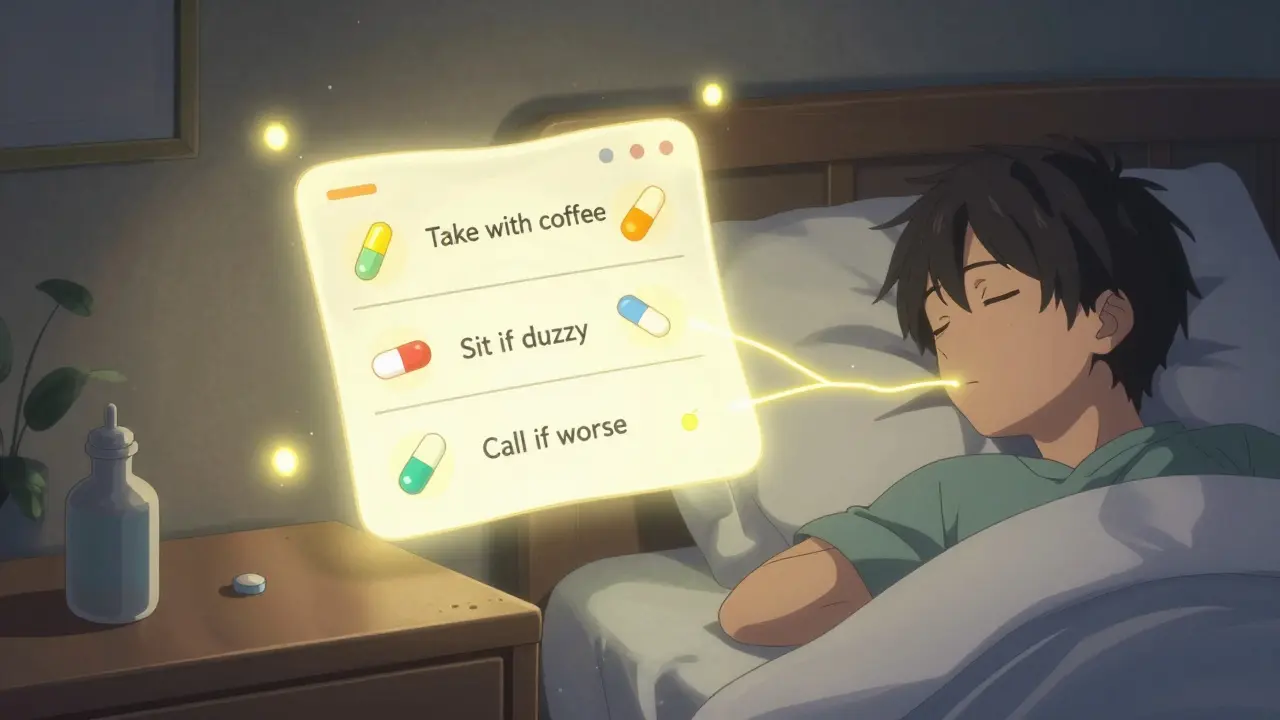
Studies show that when patients actively help create their own plan, medication adherence jumps by 25% to 40%. That means fewer missed doses, fewer ER visits, and fewer hospital stays. One 2021 survey of 12,500 Medicare beneficiaries found that 70% said having a written plan reduced their confusion about when to take each pill. But not all plans are created equal. A Johns Hopkins study found that patients given generic, pre-printed plans saw no improvement at all. The difference? Personalization. The best plans don’t just list meds-they match your life. If you forget pills because you don’t eat breakfast, the plan might say: “Take your blood pressure pill with your afternoon coffee.” If you’re scared of dizziness from a new drug, it might say: “If you feel lightheaded after taking this, sit down for 10 minutes. Call your doctor if it happens twice in one week.”Who’s Involved in Making the Plan?
This isn’t something you do alone. Your care team includes:- Your pharmacist: They know your full medication list, check for dangerous interactions, and spot duplicate prescriptions.
- Your doctor: They decide what you need and why, and adjust doses based on how you’re doing.
- Your nurse or care coordinator: They help you understand the plan and connect you to resources.
- You: You’re the most important person here. Only you know your routine, your fears, and what actually works.
How to Prepare for Your Medication Action Plan Meeting
Don’t walk into your appointment with just your memory. Bring everything:- All prescription bottles (even empty ones)
- All over-the-counter pills, patches, creams, or liquids
- Vitamins, supplements, and herbal remedies
- A list of any medicines you stopped taking and why
- Your questions written down
- “Which of these are absolutely necessary?”
- “Is there a cheaper version that works just as well?”
- “What happens if I skip one dose?”
- “What side effects should I never ignore?”
- “Can any of these interact with my food, alcohol, or other meds?”

What Goes Into a Real Medication Action Plan?
A good plan has five key parts:- A complete list: Every medication you take, including name, dose, frequency, and reason. No guessing.
- Clear action steps: Not “take as directed.” Instead: “Take 10 mg of lisinopril every morning with breakfast. If you forget, take it as soon as you remember-but never double up.”
- Visual aids: Color-coded tabs (blue for heart meds, green for diabetes), pictures of pills, or a weekly chart showing AM/PM doses.
- “If-then” scenarios: “If you feel dizzy after taking your blood pressure pill, lie down. If it happens more than once a week, call your doctor.”
- Measurable goals: “I will take all my morning pills correctly for 28 days in a row.” Then you track it.
What to Avoid in a Medication Action Plan
Bad plans share common flaws:- Using medical jargon like “hypertension” instead of “high blood pressure.”
- Listing meds without explaining why you take them.
- Ignoring your daily routine. A plan that says “take at bedtime” won’t work if you’re awake until 2 a.m.
- Being too vague. “Take as prescribed” is useless.
- Not updating it. If you stop a pill or add a new one, the plan must change.
Keeping Your Plan Alive
A Medication Action Plan isn’t a one-time thing. It’s a living document. Update it:- Every time you start or stop a medication
- After every doctor’s visit
- When you move, change pharmacies, or switch insurance
- At least every three months, even if nothing changed