When you take clindamycin for a tooth infection, a skin abscess, or a respiratory bug, you expect it to help. But what you might not know is that even one pill can set off something dangerous inside your gut - a clindamycin-linked infection called Clostridioides difficile, or C. diff. It’s not rare. It’s not just for hospital patients. And if you ignore the early signs, it can turn life-threatening in days.
Why Clindamycin Is Different
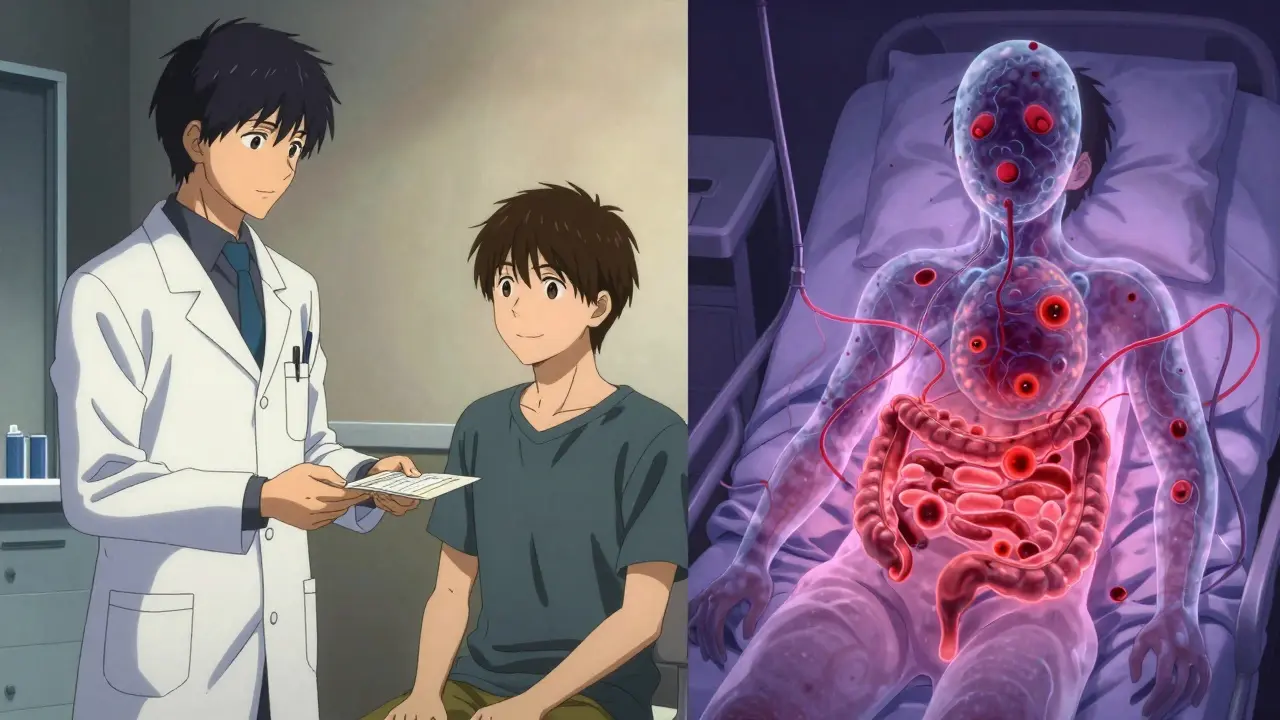
Not all antibiotics are created equal when it comes to gut damage. Clindamycin stands out because it doesn’t just kill the bad bacteria - it wipes out the good ones too. While most antibiotics target a broad range of microbes, clindamycin zeroes in on gram-positive bacteria, which includes many of the helpful bugs that keep your gut balanced. This creates a vacuum. And in that vacuum, C. diff - a tough, spore-forming bacterium - takes over. Studies show clindamycin carries the highest risk of causing C. diff among all commonly used antibiotics. One analysis of over 150,000 patients found clindamycin was linked to more cases of C. diff than fluoroquinolones, cephalosporins, or even vancomycin. Even a single dose - like the one given before a dental procedure - can be enough to trigger it. The CDC calls it an "urgent threat," and for good reason: it’s responsible for nearly a quarter of all antibiotic-related diarrhea cases in the U.S.What C. diff Actually Does
C. diff doesn’t just cause loose stools. It produces toxins that attack the lining of your colon. This leads to inflammation, ulcers, and in severe cases, a life-threatening condition called toxic megacolon. The bacteria form spores that survive handwashing, cleaning products, and even stomach acid. Once they’re in your gut, they wait - sometimes for weeks - before activating. The average time between starting clindamycin and noticing symptoms is 5 to 10 days. But it can happen as early as day one or as late as 12 weeks after you’ve finished the course. That’s why people often miss the connection. They think, "I’m not on the antibiotic anymore, so it can’t be that." But the damage lingers.When to Worry: The Red Flags
You don’t need to wait for a medical textbook to tell you something’s wrong. Here’s what to watch for - especially if you’ve taken clindamycin in the last 12 weeks:- Three or more loose or watery stools in a single day, for two days or more
- Abdominal cramping or pain that’s worse than normal gas
- Fever over 101.3°F (38.5°C)
- Blood or pus in your stool
- Nausea, vomiting, or loss of appetite
- Signs of dehydration: dizziness, dry mouth, very little urine, or dark yellow urine
What Happens If You Delay
C. diff doesn’t wait. The longer you wait to get checked, the worse it gets. A 2022 study from the University of Michigan found patients who waited more than 72 hours after symptoms started were more than twice as likely to need surgery to remove part of their colon. Their death rate was four times higher than those who got help early. Severe cases can lead to:- Low blood pressure that doesn’t respond to fluids
- Paralyzed bowel (ileus) - where your gut stops moving altogether
- Perforation - a hole in the colon
Who’s at Risk - And Why
You might think C. diff only happens in hospitals. But nearly half of all cases now start in the community. That means your dentist’s prescription for clindamycin after a root canal, or your doctor giving it for a sinus infection, could be the trigger. People most at risk:- Older adults (especially over 65)
- Those who’ve taken antibiotics recently - even one dose
- People with prior C. diff infections
- Those on proton pump inhibitors (like omeprazole)
- Patients with kidney disease or weakened immune systems
What Doctors Do - And What You Should Ask
If you go in with symptoms, your doctor will likely order a stool test for C. diff toxins. If it’s positive, treatment starts immediately. The first-line drugs are vancomycin or fidaxomicin. Fidaxomicin is more expensive but has a lower chance of recurrence - about 15% compared to vancomycin’s 25%. But here’s the key question you should ask your doctor: "Is there a safer antibiotic I could have taken?" For skin infections, trimethoprim-sulfamethoxazole is often just as effective as clindamycin - and carries far less C. diff risk. For dental infections, amoxicillin is usually the go-to, unless you’re allergic. If you’re allergic to penicillin, ask about azithromycin or metronidazole instead. Clindamycin should be the last option, not the first.
What’s New in Treatment
The good news? There’s progress. In 2023, the FDA approved VOWST - a pill made from frozen, purified bacterial spores from healthy donors. It’s like a probiotic on steroids, designed to restore your gut microbiome after C. diff. Early results show it cuts recurrence rates by over 80% in people who’ve had multiple episodes. Another promising drug, ridinilazole, is in late-stage trials. In studies, it reduced recurrence by nearly half compared to vancomycin - especially in patients who’d taken clindamycin. These aren’t just lab results. They’re real tools that are changing outcomes.What You Can Do Now
If you’re currently taking clindamycin:- Don’t stop the medication unless your doctor tells you to - but watch closely for symptoms.
- Stay hydrated. Drink water, broth, or oral rehydration solutions. Avoid sugary drinks - they can make diarrhea worse.
- Don’t take over-the-counter anti-diarrhea meds like loperamide (Imodium). They trap toxins in your gut and can make things worse.
- Wash your hands with soap and water after using the bathroom. Alcohol-based hand sanitizers don’t kill C. diff spores.
- Keep monitoring for symptoms for the next 12 weeks.
- Don’t assume any new diarrhea is "just a bug."
- Keep a record: how many stools a day, color, consistency, any pain or fever.
Bottom Line
Clindamycin works. But it comes with a hidden cost. The risk of C. diff is real, serious, and often overlooked. You don’t need to avoid it completely - sometimes it’s the best tool for the job. But you do need to know the signs. You need to act fast. And you need to ask questions. If you’re on clindamycin and you start having diarrhea, cramps, or fever - don’t wait. Don’t Google it. Don’t hope it goes away. Call your doctor today. If symptoms are severe, go to the ER. Early action saves lives - and guts.Can one dose of clindamycin cause C. diff?
Yes. Even a single dose of clindamycin can trigger C. diff infection. Case reports show symptoms developing after just one pill, especially in older adults or those with prior gut issues. While the absolute risk is low (around 1-2%), the risk per dose is higher than with almost any other antibiotic.
How long after stopping clindamycin can C. diff start?
Symptoms can appear anytime from 1 day to 12 weeks after finishing clindamycin. Most cases occur within 14 days of starting the drug, and nearly half happen within a week after stopping. This long window is why many people don’t connect their diarrhea to the antibiotic they took weeks ago.
Is C. diff contagious?
Yes. C. diff spreads through spores in feces. If someone with the infection doesn’t wash their hands properly, they can contaminate surfaces, doorknobs, or medical equipment. Others can pick up the spores and swallow them. That’s why handwashing with soap and water - not just hand sanitizer - is critical in preventing spread.
Should I take probiotics to prevent C. diff?
There’s no strong evidence that over-the-counter probiotics prevent C. diff. Some strains like Saccharomyces boulardii show modest benefit in studies, but they’re not a substitute for careful antibiotic use. Don’t rely on them. The best prevention is using the right antibiotic in the first place - and knowing when to seek help.
Can C. diff come back after treatment?
Yes. About 20-30% of people who recover from C. diff will have it return, sometimes multiple times. Recurrence is more common after vancomycin treatment and in people who are older, have ongoing antibiotic use, or have weakened immune systems. New treatments like VOWST and ridinilazole are designed specifically to lower this risk.
Are there alternatives to clindamycin for dental infections?
Yes. If you’re not allergic to penicillin, amoxicillin is the first choice. If you are allergic, azithromycin or metronidazole are often safer alternatives with lower C. diff risk. Trimethoprim-sulfamethoxazole is another option for skin or soft tissue infections. Always ask your dentist or doctor if there’s a lower-risk option available.
