Ulcerative colitis isn't just about frequent bathroom trips. It’s a chronic condition where your colon’s inner lining becomes inflamed, develops open sores, and turns into a source of constant discomfort, pain, and unpredictability. Unlike a stomach bug that fades in a few days, ulcerative colitis (UC) sticks around - flaring up without warning and sometimes vanishing for months or even years. The good news? Most people with UC can live full, active lives. But only if they understand what’s happening inside their body and how to manage it properly.
What Exactly Happens in Your Colon With Ulcerative Colitis?
Ulcerative colitis attacks the large intestine - specifically the colon and rectum. It doesn’t jump around like Crohn’s disease. Instead, it starts in the rectum and moves upward in a continuous line, damaging the innermost layer of the colon wall. This isn’t just irritation. The immune system mistakenly targets the lining of the gut, causing swelling, ulcers, and bleeding. You don’t get patches of healthy tissue mixed in - if it’s affected, the entire stretch is inflamed.
There are five main types of UC, defined by how far the inflammation spreads:
- Ulcerative proctitis: Only the rectum is involved. Symptoms are often limited to rectal bleeding and a feeling of urgency.
- Proctosigmoiditis: Inflammation reaches the sigmoid colon (the lower part of the colon). You’ll likely have bloody diarrhea and cramps on the left side.
- Left-sided colitis: The inflammation goes up to the splenic flexure, near the spleen. Pain on the left side, weight loss, and more frequent bowel movements are common.
- Pancolitis: The entire colon is affected. This is the most severe form - you might have more than 10 bowel movements a day, heavy bleeding, fever, and significant weight loss.
- Rectal-sparing UC: Rare. The rectum stays healthy while the rest of the colon is inflamed.
One thing you’ll almost always have: blood in your stool. In fact, nearly every person with UC experiences this during a flare. Alongside that comes abdominal cramping, especially on the left side, and tenesmus - that awful feeling that you need to go, even when your bowels are empty.
Why Does This Happen? The Real Cause (And What Doesn’t Cause It)
No one knows exactly why ulcerative colitis starts. But we do know it’s not your fault. You didn’t eat too much junk food. You didn’t stress yourself into it. And it’s not contagious.
What’s happening is an autoimmune response. Your immune system, which is supposed to protect you from germs, turns on your own colon lining. People with UC have immune systems that misfire - they see harmless bacteria or cells in the gut as threats and launch an attack. This goes on for months, even years, causing constant damage.
Some factors increase your risk:
- Being of Caucasian or Ashkenazi Jewish descent
- Having a close family member with IBD or another autoimmune disease like psoriasis
- Being diagnosed between ages 15-30 or 50-70 - those are the two main peaks
But here’s the myth-busting part: food and stress don’t cause ulcerative colitis. They can trigger a flare, sure. A big party, a stressful work deadline, or eating spicy food might make symptoms worse. But they didn’t start the disease. That’s important to understand - blaming yourself makes it harder to focus on real management.
What Does a Flare Feel Like? Real Symptoms Beyond Diarrhea
Flares aren’t all the same. Some start slowly - a few extra trips to the bathroom, a little blood in the toilet, mild cramps. Others hit like a storm: high fever, violent diarrhea with mucus and blood, severe pain, and even vomiting.
People with pancolitis often describe their stool as almost entirely blood and pus. Those with ulcerative proctitis might only notice bright red blood after a bowel movement and feel like they can’t fully empty their bowels. Both are valid forms of UC - just different in severity.
And it’s not just your gut. About one in three people with UC develop problems outside the digestive tract:
- Red, itchy, or painful eyes (uveitis or episcleritis)
- Joint pain, especially in the knees, ankles, or wrists
- Skin rashes or painful lumps (erythema nodosum or pyoderma gangrenosum)
- Fatigue so deep it doesn’t go away with sleep
These extraintestinal symptoms can be the first sign of UC - sometimes even before digestive issues appear. That’s why doctors need to look at the whole picture.
How Do You Know It’s UC and Not Crohn’s Disease?
People often confuse ulcerative colitis with Crohn’s disease. Both are types of inflammatory bowel disease, but they’re very different.
UC only affects the colon and rectum. Crohn’s can show up anywhere - mouth to anus. UC only damages the inner lining. Crohn’s eats through all layers of the bowel wall. UC’s inflammation is continuous. Crohn’s leaves patches of healthy tissue between inflamed areas - called "skip lesions."
Testing helps clear it up. A colonoscopy with biopsies is the gold standard. Imaging and blood tests rule out infections or other conditions. Getting the right diagnosis changes everything - because treatments aren’t always interchangeable.
How to Get Into and Stay in Remission
Remission isn’t just "feeling better." It means the inflammation has gone down, ulcers have healed, and you’re not having bloody stools or constant cramps. The goal is long-term remission - months or years without symptoms.
Medication is the foundation. Here’s how it usually works:
- Mild cases: 5-aminosalicylates (5-ASAs) like mesalamine. These are anti-inflammatory drugs taken as pills, suppositories, or enemas. They target the colon directly.
- Moderate to severe cases: Immunosuppressants like azathioprine or 6-MP. These calm the immune system over time. They take weeks to work, so they’re often used with faster-acting drugs.
- Severe or treatment-resistant cases: Biologics. These are injectable or IV drugs that block specific parts of the immune response - like TNF-alpha (infliximab, adalimumab) or integrins (vedolizumab). Many people achieve deep remission with these.
Some people need surgery. If medications fail, or if there’s a high risk of colon cancer (especially with pancolitis), removing the entire colon and rectum (colectomy) can cure UC. After surgery, most people live without symptoms - though they’ll need an ileostomy or a pouch built from the small intestine.
Remission isn’t just about pills. Lifestyle matters too:
- Track your triggers: Keep a food and symptom journal. Common triggers include dairy, spicy foods, caffeine, and alcohol - but yours might be different.
- Eat during flares: When your gut is inflamed, high-fiber foods can make things worse. Stick to low-residue foods like white rice, bananas, cooked vegetables, and lean protein. Hydration is critical - diarrhea drains fluids fast.
- Manage stress: While stress doesn’t cause UC, it can make flares worse. Yoga, meditation, therapy, or even regular walks help.
- Get screened: People with pancolitis for more than 8-10 years have a higher risk of colon cancer. Regular colonoscopies every 1-2 years are essential.
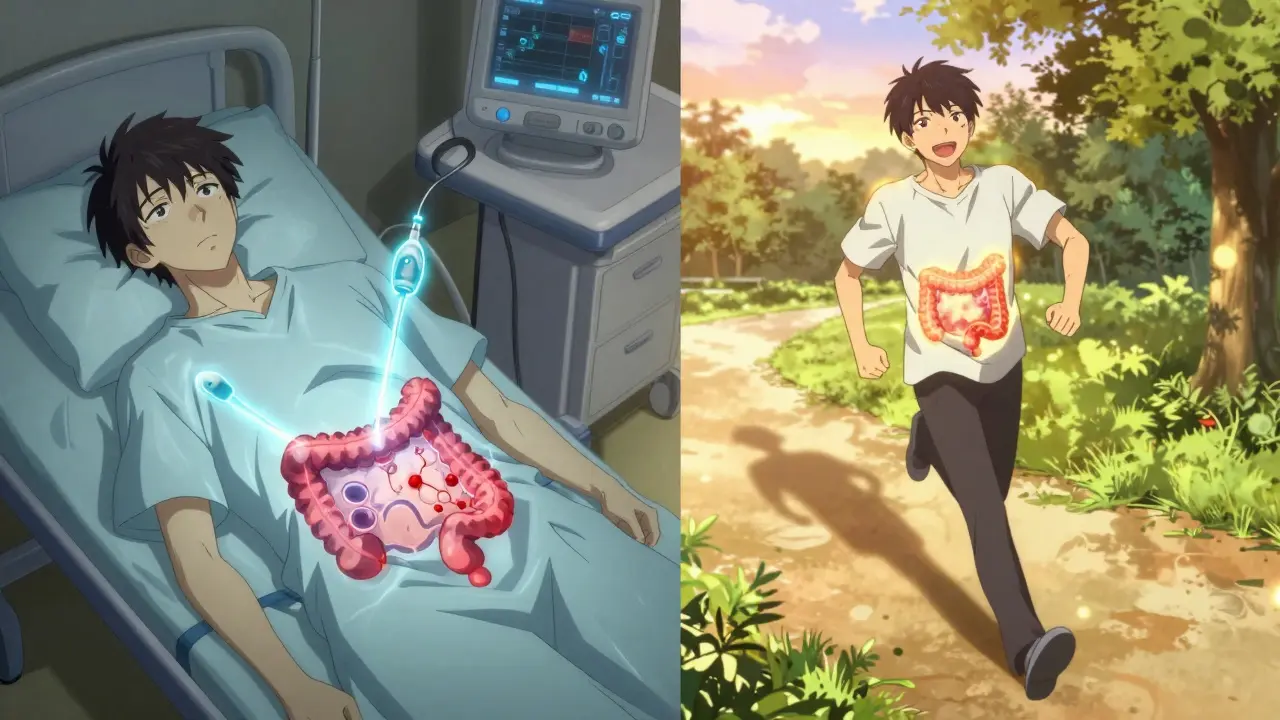
What to Expect Long-Term: Can You Live a Normal Life?
Yes. Most people with UC do.
It’s not easy. There will be bad days. You might miss work, cancel plans, or feel embarrassed. But with the right treatment plan, many people go years without a flare. Some return to running marathons. Others raise kids, travel, or start businesses.
The key is consistency. Taking your meds even when you feel fine. Going to follow-up appointments. Talking to your doctor when things change - not waiting until you’re in crisis.
And you’re not alone. In the UK, tens of thousands live with UC. Support groups, online forums, and patient advocacy organizations offer real advice and emotional support. You don’t have to figure it out by yourself.
When to Call Your Doctor
Don’t wait. Call your gastroenterologist if you notice:
- More than six bloody bowel movements in a day
- Fever over 38°C (100.4°F) that doesn’t go away
- Severe abdominal pain or swelling
- Signs of dehydration - dizziness, dark urine, dry mouth
- Sudden weight loss without trying
These could mean your UC is worsening or you have a complication like toxic megacolon or severe infection. Early action saves lives.
Can ulcerative colitis be cured?
There’s no medical cure for ulcerative colitis - but there is a surgical one. Removing the entire colon and rectum (colectomy) stops the disease permanently. For most people, however, UC is managed long-term with medication, diet, and lifestyle changes. Many achieve deep, lasting remission and live full lives without surgery.
Do I need to avoid all fiber if I have UC?
Not always. During a flare, high-fiber foods like raw vegetables, nuts, seeds, and whole grains can worsen cramping and diarrhea. But when you’re in remission, gradually adding fiber back in can help gut health. Soluble fiber - like oats, bananas, and peeled apples - is usually better tolerated than insoluble fiber. Always adjust based on your symptoms.
Can I still drink alcohol with ulcerative colitis?
Many people find alcohol triggers flares - especially beer and wine. Alcohol irritates the gut lining and can interfere with medications. While some people tolerate small amounts during remission, others need to avoid it completely. The safest approach is to eliminate it and test slowly if you want to reintroduce it later.
Is ulcerative colitis the same as IBS?
No. Irritable bowel syndrome (IBS) affects how the bowel functions but doesn’t cause inflammation or damage to the tissue. UC involves real, visible inflammation and ulcers. IBS doesn’t increase cancer risk. UC does. Blood in stool, fever, and weight loss are signs of UC - not IBS. They’re treated completely differently.
Can children get ulcerative colitis?
Yes. While UC often appears between ages 15-30, it can develop in children too. Pediatric UC can affect growth and development, so early diagnosis and treatment are critical. Kids may need different dosing or monitoring plans, but the same principles apply: control inflammation, prevent flares, and support quality of life.
What’s the risk of colon cancer with UC?
The longer you have pancolitis (inflammation of the whole colon), the higher your risk - especially after 8-10 years. People with ulcerative proctitis have almost no increased risk. Regular colonoscopies with biopsies are the best way to catch early changes. If dysplasia (pre-cancerous cells) is found, your doctor may recommend surgery to remove the colon.
Next Steps: What to Do Today
If you’ve just been diagnosed:
- Write down your symptoms - how often you go, what your stool looks like, any pain or fatigue.
- Ask your doctor about your specific type of UC and what your treatment plan looks like.
- Start a symptom journal - even just a simple notes app on your phone.
- Find a dietitian who specializes in IBD. They can help you eat well without triggering flares.
- Join a support group. Talking to others who get it reduces isolation.
If you’ve had UC for years:
- Are you still on your original meds? Many people need adjustments over time.
- When was your last colonoscopy? Don’t skip screenings.
- Are you feeling emotionally drained? Mental health support is part of UC care.
Ulcerative colitis is lifelong - but it doesn’t have to define you. With the right tools, support, and knowledge, you can control it. Not just survive. Thrive.
