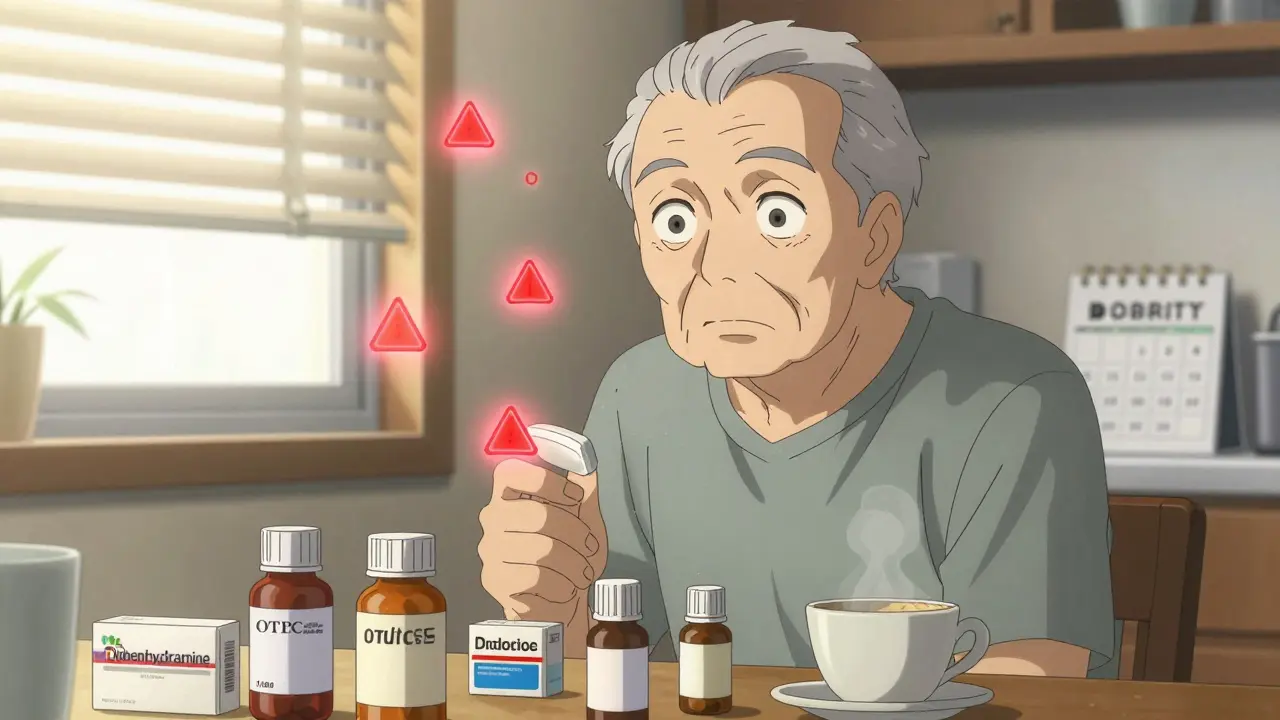
More than 1 in 3 adults over 65 in the U.S. take five or more medications every day. That’s not unusual - it’s normal for people managing multiple health conditions. But here’s the hidden danger: many of them are accidentally taking the same active ingredient twice. And that can land them in the hospital.
Imagine this: you take a prescription painkiller for your arthritis. It contains acetaminophen. Then you grab a cold medicine from the shelf because you’ve got a stuffy nose. It also contains acetaminophen. You don’t think twice - you’re just trying to feel better. But by the end of the day, you’ve taken more than double the safe daily limit. Your liver starts to struggle. Within hours, you’re in the ER with liver damage. This isn’t rare. It happens tens of thousands of times a year.
Why Double Ingredients Are So Dangerous
The problem isn’t just about taking too many pills. It’s about taking too much of the same chemical. The body doesn’t care if the acetaminophen comes from a brand-name pill, a generic, or a cold syrup. It only sees the dose. The safe limit for acetaminophen is 3,000 to 4,000 milligrams per day for most adults. But if you’re taking two or three products that each contain 500 mg, you can hit that limit without realizing it.
Acetaminophen is the most common offender, but it’s not the only one. Diphenhydramine - the sleepy-making ingredient in Benadryl - shows up in sleep aids, allergy pills, and even some cough syrups. Pseudoephedrine, a decongestant, hides in multiple cold and flu formulas. NSAIDs like ibuprofen and naproxen are in pain relievers, arthritis meds, and even some topical gels. When you stack them, you risk stomach bleeding, kidney damage, or extreme drowsiness.
Older adults are especially at risk. The CDC says 65% of hospitalizations from double ingredient errors happen to people 65 and older. Why? Because they’re more likely to see multiple doctors, fill prescriptions at different pharmacies, and use OTC meds without telling anyone. And many don’t realize their “natural” supplements or herbal remedies might contain hidden drugs.
How You’re Getting Hit Without Knowing It
You’re not being careless. The system is designed to confuse you.
Prescription labels rarely mention if the drug has the same active ingredient as something you bought over the counter. A 2022 FDA review found that 45% of prescription labels don’t clearly warn about overlaps. OTC labels? They’re better since the FDA updated the Drug Facts format in 2020 - but 41% of people still can’t find or understand the active ingredient section, according to a 2023 Government Accountability Office report.
And then there’s the pharmacy problem. If you fill your prescriptions at Walgreens one month and CVS the next, those systems don’t talk to each other. A 2021 JAMA study showed that using one pharmacy cuts double ingredient risks by 63%. Why? Because that single pharmacy’s software flags duplicates across all your meds - including OTCs you’ve bought there before.
Even your doctor might not know. A 2021 study in the Journal of the American Geriatrics Society found that 67% of older adults who had a double ingredient incident said their provider never asked about the OTC medicines they were taking. That’s not negligence - it’s a gap in the system. Most electronic health records don’t track OTC use unless you tell them, and most patients don’t think to mention it.
The Real Culprits: Cold, Allergy, and Pain Meds
Let’s get specific. The top three troublemakers are:
- Cold and flu medicines - 73% of double ingredient cases involve these. Products like Tylenol Cold, NyQuil, DayQuil, and store-brand equivalents often contain acetaminophen, dextromethorphan, and pseudoephedrine. Taking one of these while also on a prescription painkiller? High risk.
- Allergy meds - Benadryl, Zyrtec, Claritin, and their generics all have different active ingredients, but many people assume they’re safe to mix. Some allergy meds also contain sedatives like diphenhydramine, which can dangerously amplify the effect of prescription sleep aids or anti-anxiety drugs.
- Pain relievers - If you’re taking a prescription opioid like oxycodone or hydrocodone, it likely already includes acetaminophen. Adding Extra Strength Tylenol? You’re doubling down on liver stress. Same goes for NSAIDs - if you’re on a prescription naproxen for back pain, don’t also take Aleve.
And don’t forget the “natural” stuff. Some herbal supplements - like St. John’s Wort or kava - can interact with prescription meds. Others, like certain Chinese herbal formulas, have been found to contain hidden NSAIDs or steroids. A 2019 WHO report says 68% of patients don’t tell their doctors about these, thinking they’re harmless.

What You Can Do Right Now
You don’t need a PhD in pharmacology to protect yourself. Here’s what works, based on real data from the CDC, NCCMERP, and top medical groups:
- Make a complete list of everything you take - every pill, capsule, patch, liquid, cream, and supplement. Include brand names, generic names, doses, and how often you take them. Write it down. Don’t rely on memory.
- Keep it with you - Put a copy in your wallet, your purse, or your phone. Emergency responders need to see it. So do your doctors.
- Use one pharmacy - If you’re filling prescriptions at multiple places, stop. Pick one. Their system will flag duplicates, even if you bought the OTC stuff there last year.
- Ask your pharmacist every time - When you get a new prescription, say: “Can this interact with anything else I’m taking?” They’re trained to catch this stuff. Pharmacy Times reports they identify double ingredient risks in 87% of medication reviews.
- Read the Drug Facts label - On every OTC box, find the “Active Ingredients” section. It’s usually at the top. If you see the same name on two different products, don’t take them together.
- Have a full med review once a year - Bring your list to your primary doctor. Ask: “Which of these do I still need?” The American Geriatrics Society’s Beers Criteria® lists 30 high-risk combinations - your doctor should know them.
What’s Changing to Fix This
Things are improving - slowly. The FDA’s new Drug Facts label rules (full compliance by 2025) will make active ingredients easier to spot. Apple Health on iOS 17 now warns you if you’re adding a new OTC med that duplicates something you’ve already entered. Epic and Cerner, the two biggest electronic health record systems, now have built-in double ingredient alerts that work 92% of the time - if the OTC meds are entered.
Medicare Part D plans now use a quality measure called the Drug-Drug Interactions metric, which has cut senior hospitalizations from double ingredient errors by 28% since 2021. And new tools like MedWise Risk Score use AI to scan your full med list and give you a risk rating - 89% accurate, according to its developers.
But technology alone won’t fix this. The real solution is you - knowing your meds, asking questions, and speaking up.
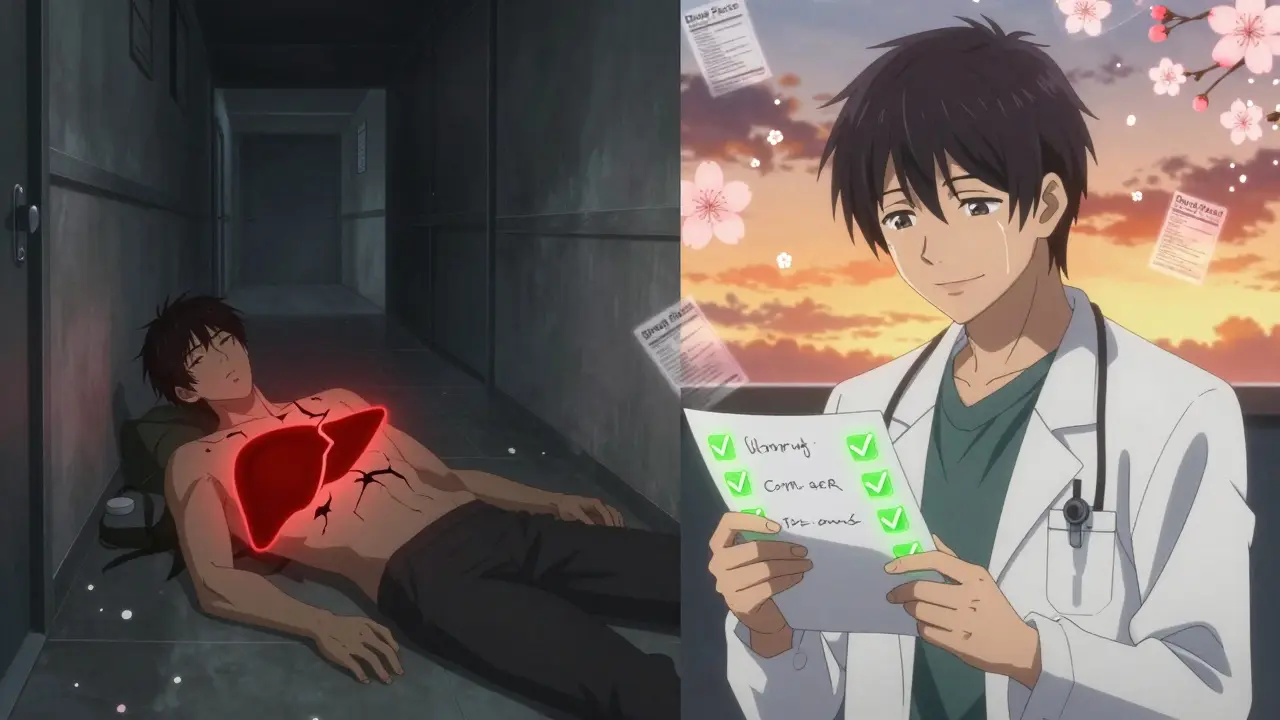
What to Do If You’ve Already Taken Too Much
If you suspect you’ve taken too much acetaminophen, don’t wait for symptoms. Call Poison Control at 1-800-222-1222 immediately. Liver damage from acetaminophen can happen without nausea or pain in the early stages. The sooner you get treatment - usually with N-acetylcysteine - the better your chances.
For other overdoses - like too much diphenhydramine causing extreme drowsiness, or pseudoephedrine causing high blood pressure - go to the ER. Don’t try to sleep it off. Don’t wait until morning. Double ingredient reactions can escalate fast.
Final Thought: It’s Not About Taking Fewer Pills - It’s About Taking the Right Ones
People think polypharmacy means “too many meds.” But the real issue isn’t quantity. It’s duplication. You might need all five pills. But you don’t need two of them to have the same chemical. That’s where the harm happens.
Take control. Write it down. Talk to your pharmacist. Use one pharmacy. Ask the same question every time: “Could this be the same as something else I’m taking?”
It’s not complicated. It just takes a little attention. And that attention could save your liver, your kidneys, or even your life.
How do I know if two medications have the same active ingredient?
Look at the "Active Ingredients" section on the Drug Facts label of any over-the-counter medicine. For prescriptions, check the pill bottle or ask your pharmacist. Common ones to watch for: acetaminophen (Tylenol), diphenhydramine (Benadryl), pseudoephedrine (Sudafed), ibuprofen (Advil), and naproxen (Aleve). If the same name appears on two different products, don’t take them together.
Can I trust my doctor to catch double ingredients?
Not always. Studies show that 67% of older adults who had a double ingredient incident said their doctor never asked about over-the-counter meds. Doctors are busy, and most electronic records don’t track OTC use unless you tell them. That’s why you need to bring your own list - every visit.
Is it safe to take OTC meds with my prescriptions?
Only if you check first. Many OTC products contain ingredients that overlap with prescriptions - especially painkillers, cold meds, and sleep aids. Even something as simple as a nighttime allergy pill can contain a sedative that adds up dangerously with your anxiety or sleep medication. Always ask your pharmacist before combining them.
Why does using one pharmacy help?
Because that pharmacy’s system can see everything you’ve bought there - prescriptions and OTCs. Their software flags duplicates automatically. When you use multiple pharmacies, each one only sees its own records. A 2021 JAMA study found that using one pharmacy reduces double ingredient errors by 63%.
What should I do if I think I’ve taken too much acetaminophen?
Call Poison Control at 1-800-222-1222 right away. Don’t wait for symptoms like nausea or pain. Liver damage from acetaminophen can start without warning. If you can’t reach them, go to the ER. Early treatment with N-acetylcysteine can prevent serious harm.
Are herbal supplements safe to take with my other meds?
Not necessarily. Some herbal products contain hidden drugs - like NSAIDs or steroids - that aren’t listed on the label. Others, like St. John’s Wort, can interfere with how your body processes prescription meds. Always tell your doctor and pharmacist about every supplement you take, even if you think it’s "natural."