Gut Microbiome Risk Calculator
Personalized Gut Health Risk Assessment
Calculate your risk of microbiome disruption from esomeprazole based on clinical evidence. The tool uses data from the latest studies on PPI effects.
Risk Assessment
Everyone’s heard the warning that long‑term use of acid‑blocking drugs can stir up trouble in the gut, but what does the science really say about esomeprazole and the bacteria living in our intestines? This article pulls together the latest clinical data, explains the mechanisms that link a powerful proton pump inhibitor (PPI) to changes in microbial balance, and offers practical tips for anyone who needs to stay on the medication without sacrificing gut health.
What is Esomeprazole?
Esomeprazole is a second‑generation proton pump inhibitor (PPI) that reduces gastric acid secretion by irreversibly blocking the H+/K+‑ATPase enzyme in stomach parietal cells. Marketed under the brand name Nexium, it was approved by the FDA in 2001 and quickly became a go‑to treatment for gastro‑esophageal reflux disease (GERD), peptic ulcers, and Zollinger‑Ellison syndrome. Because it is the S‑enantiomer of omeprazole, it provides more consistent plasma levels and a slightly longer half‑life, which translates to better symptom control for many patients.
Understanding the Gut Microbiome
Gut microbiome refers to the trillions of bacteria, archaea, viruses, and fungi that colonize the gastrointestinal tract. This ecosystem is dominated by two bacterial phyla-Bacteroidetes and Firmicutes-which together regulate digestion, immune function, and even mood. When the balance shifts, a condition known as dysbiosis can arise, leading to inflammation, nutrient malabsorption, and higher susceptibility to infections.
How PPIs Alter the Microbial Landscape
Proton pump inhibitors raise gastric pH from the usual 1‑2 up to 4‑5. That sounds harmless, but the stomach’s acidity is a primary defense against ingested microbes. When the barrier weakens, more bacteria survive the journey to the intestines, reshaping the community composition. A 2023 meta‑analysis of 42 observational studies found that PPI users had a 2.2‑fold higher odds of developing dysbiosis, with a notable rise in oral‑origin bacteria such as Streptococcus and Veillonella. The effect is dose‑dependent; higher daily doses of esomeprazole correlate with larger shifts in bacterial diversity.
Key Microbiome Changes Linked to Esomeprazole
| Parameter | Esomeprazole users | Non‑PPI controls |
|---|---|---|
| Alpha diversity (Shannon index) | ↓ 15% on average | Baseline |
| Relative abundance of Firmicutes | ↑ 20% | Stable |
| Relative abundance of Bacteroidetes | ↓ 12% | Stable |
| Oral‑origin taxa (Streptococcus, Veillonella) | ↑ 3‑5‑fold | Rare |
| Clostridioides difficile colonization | ↑ 1.8‑fold risk | Baseline risk |
| Short‑chain fatty acid (SCFA) production | ↓ 10% but variable | Normal range |
These numbers illustrate two consistent themes: reduced microbial diversity and a tilt toward taxa that thrive in less acidic environments. The decline in SCFA‑producing bacteria-particularly those from the Firmicutes family that generate butyrate-has downstream implications for intestinal barrier integrity and inflammation.
Clinical Consequences of PPI‑Induced Dysbiosis
When the gut microbiome is disturbed, several health issues can surface:
- Clostridioides difficile infection (CDI): PPIs are one of the strongest modifiable risk factors for CDI. A 2022 cohort study of 150,000 hospital patients showed that esomeprazole users had a 1.7‑fold higher incidence of CDI compared with non‑users, even after adjusting for antibiotics.
- Small‑intestinal bacterial overgrowth (SIBO): Higher gastric pH encourages bacterial proliferation in the duodenum, leading to bloating, malabsorption, and chronic fatigue.
- Metabolic effects: Shifts in Firmicutes vs. Bacteroidetes ratios have been linked to insulin resistance and weight gain, although causality remains under investigation.
- Immune modulation: Reduced SCFA levels can impair regulatory T‑cell function, potentially aggravating autoimmune conditions such as IBD.

Who Is Most at Risk?
Not every esomeprazole user will develop dysbiosis, but several factors amplify the risk:
- Long‑term therapy (> 6 months) or high daily doses (≥ 40 mg).
- Concurrent antibiotic use, which already disrupts gut flora.
- Age over 65, where baseline microbiome diversity is lower.
- Existing gastrointestinal disorders like IBS or IBD.
- Genetic variants in the CYP2C19 enzyme that slow esomeprazole metabolism, leading to higher systemic exposure.
Balancing Acid‑Control Needs with Microbiome Health
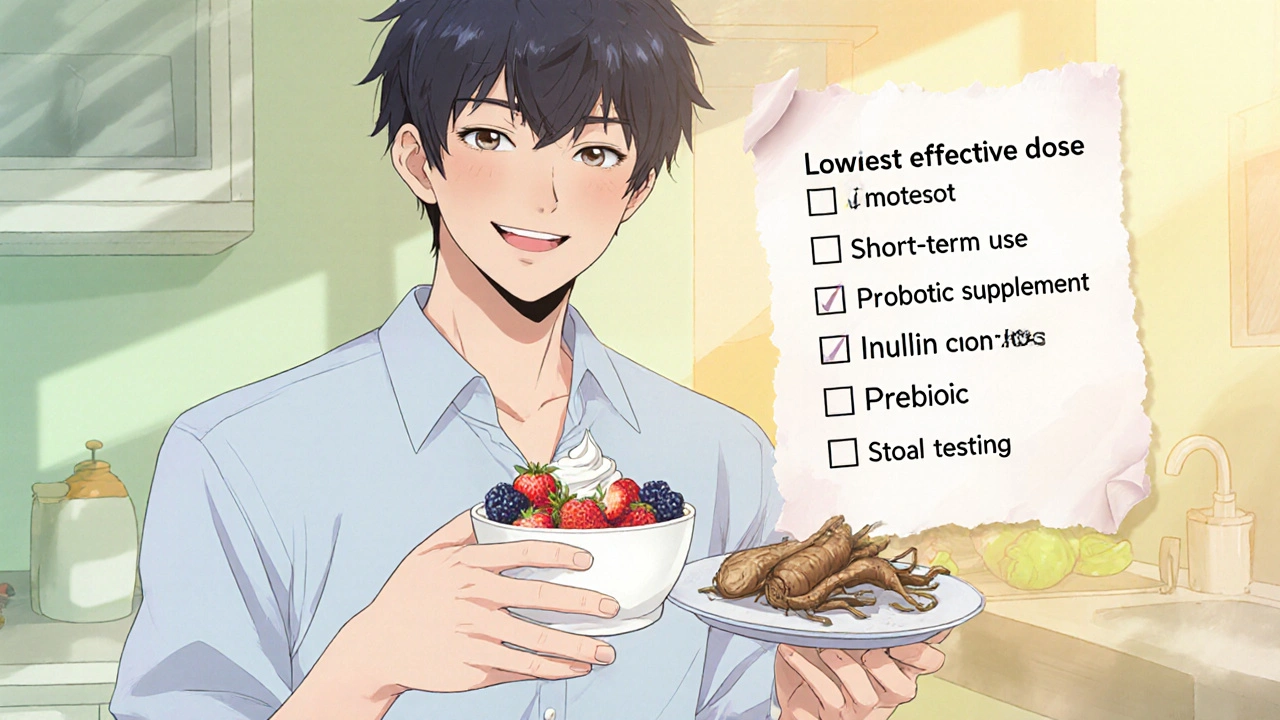
If you’ve been prescribed esomeprazole, you don’t have to ditch it outright. Here’s a practical checklist to protect your gut while still managing reflux:
- Use the lowest effective dose: Work with your physician to step down to 20 mg or switch to an on‑demand regimen once symptoms are controlled.
- Limit treatment duration: Aim for a trial of 8‑12 weeks, then reassess the need for continuation.
- Probiotic supplementation: Choose strains with documented resilience to low‑acid environments, such as Lactobacillus rhamnosus GG and Bifidobacterium lactis. Clinical trials in 2024 showed a 30% reduction in SIBO symptoms when combined with PPIs.
- Prebiotic fiber intake: Foods rich in inulin (chicory root, Jerusalem artichoke) feed butyrate‑producing bacteria and help restore SCFA levels.
- Periodic microbiome testing: Stool DNA panels can reveal overgrowth of oral‑origin taxa or early CDI colonization, allowing timely intervention.
For patients with a history of CDI, many gastroenterologists now recommend alternative reflux therapies such as H2‑blockers (e.g., ranitidine) or lifestyle modifications before resorting to PPIs.
Future Research Directions
Scientists are still untangling the exact pathways through which esomeprazole shapes the gut ecosystem. Ongoing studies focus on:
- Metabolomic profiling to track SCFA changes in real‑time.
- Longitudinal cohorts that monitor microbiome recovery after PPI discontinuation.
- Genetic sub‑analyses of CYP2C19 polymorphisms to personalize dosing.
- Development of “microbiome‑friendly” PPIs that retain acid suppression without drastic pH elevation.
Until these next‑generation drugs hit the market, the best defense remains informed prescribing and proactive gut care.
Take‑away Summary
Esomeprazole is a highly effective PPI, but its ability to raise stomach pH can disturb the delicate balance of the gut microbiome. The resulting dysbiosis may increase the risk of infections like C. difficile, promote SIBO, and subtly shift metabolic pathways. Patients can mitigate these effects by using the lowest effective dose, limiting therapy length, adding targeted probiotics and prebiotic foods, and monitoring gut health with stool tests. Discuss any concerns with a healthcare provider-sometimes a slight tweak in dosing or a switch to an H2‑blocker can preserve both acid control and microbiome integrity.
Can short‑term esomeprazole use affect the gut microbiome?
Yes. Even a 4‑week course can raise gastric pH enough to let oral bacteria colonize the intestine, causing a modest but measurable drop in microbial diversity. The changes usually revert after discontinuation, though individual recovery rates vary.
Are probiotics effective for PPI‑related dysbiosis?
Clinical trials from 2022‑2024 suggest that multi‑strain probiotics, especially those containing Lactobacillus rhamnosus GG and Bifidobacterium lactis, can reduce SIBO symptoms by roughly 30% and lower the incidence of C. difficile colonization when taken alongside a PPI.
Should I stop esomeprazole if I develop gut issues?
Do not stop abruptly without consulting a doctor. A gradual taper or switch to an H2‑blocker may relieve symptoms while preventing rebound acid hypersecretion. Your clinician can also order stool testing to determine if a specific infection needs treatment.
How does CYP2C19 affect esomeprazole’s impact on the microbiome?
People with reduced‑function CYP2C19 alleles metabolize esomeprazole more slowly, leading to higher plasma concentrations and a more pronounced rise in gastric pH. This amplifies the risk of dysbiosis, so genotype‑guided dosing is becoming a topic of research.
Is there a “microbiome‑friendly” alternative to esomeprazole?
As of 2025, no PPI has been proven to be completely microbiome‑neutral. H2‑blockers and lifestyle changes (elevating head of the bed, weight loss, avoiding trigger foods) are the main alternatives for patients who cannot tolerate PPIs.
