Antidepressant Class Selector
Select a class and click "Show Details" to learn more about its mechanism, typical drugs, onset of action, and common side effects.
Key Takeaways
- Antidepressant medications are the cornerstone of pharmacologic treatment for Major Depressive Disorder (MDD).
- Different classes act on serotonin, norepinephrine, dopamine, or multiple pathways, influencing speed of relief and side‑effect profile.
- Guidelines (e.g., NICE, APA) recommend starting with a selective serotonin reuptake inhibitor (SSRI) for most patients, adjusting based on response and tolerability.
- Common side effects include gastrointestinal upset, sexual dysfunction, weight change, and sleep disturbances; most are dose‑dependent and often improve over time.
- Monitoring for suicide risk, withdrawal syndrome, and drug interactions is essential throughout treatment.
When you or a loved one receives a diagnosis of Major Depressive Disorder is a mood disorder marked by persistent sadness, loss of interest, and impaired daily functioning lasting at least two weeks, the first question is usually - what will help the mood lift? Antidepressant medications are the most widely prescribed drug group for MDD, and they work by correcting chemical imbalances that underlie depressive symptoms. This guide walks through how these drugs act, when they’re used, the main classes you’ll hear about, and practical tips for staying safe and getting the best results.
How Antidepressants Work: The Basic Biology
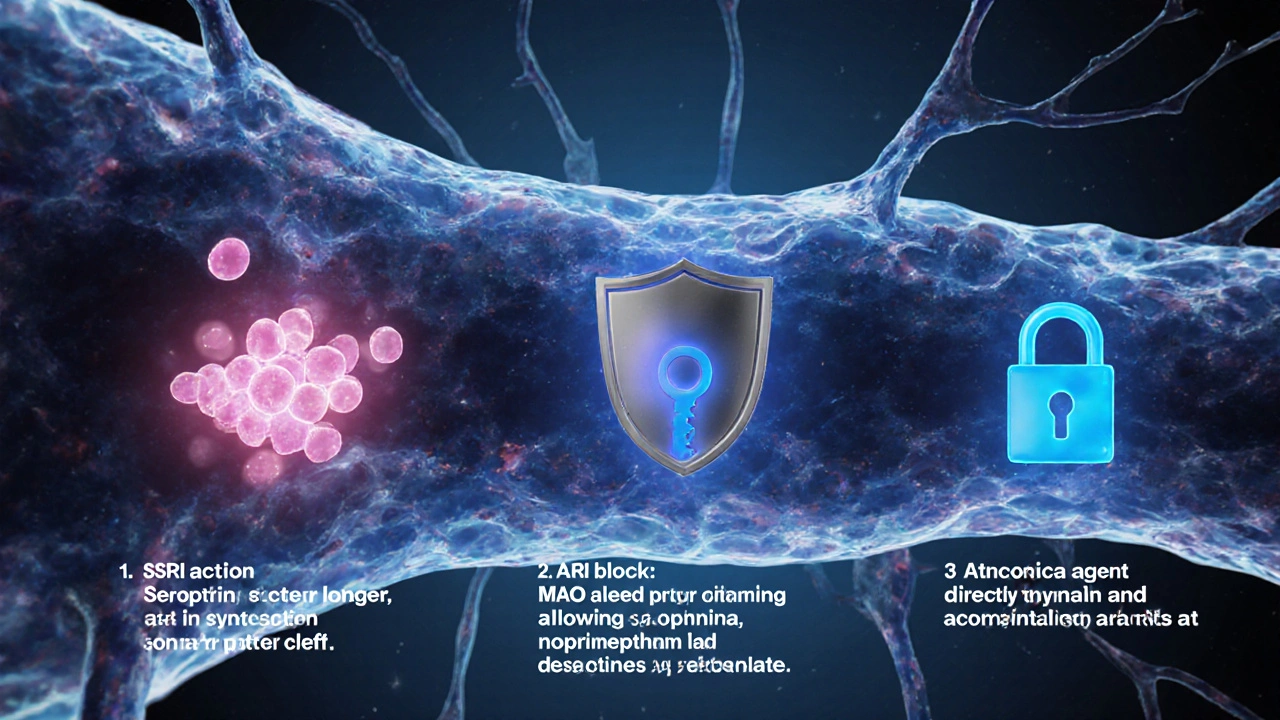
Brain cells (neurons) communicate via neurotransmitters - chemical messengers like serotonin, norepinephrine, and dopamine. In depression, the levels or activity of these messengers can be too low or the receptors become less responsive. Antidepressants boost neurotransmission in one of three ways:
- Prevent re‑uptake of a neurotransmitter so it stays in the synaptic gap longer (most SSRIs and SNRIs).
- Block the enzyme that breaks down neurotransmitters (MAOIs).
- Directly stimulate receptors or alter their sensitivity (some atypical agents).
By increasing the availability of mood‑regulating chemicals, symptoms such as sadness, fatigue, and hopelessness often improve within weeks.
Major Classes of Antidepressant Medications
Each class has a distinct mechanism, common drugs, and a characteristic side‑effect pattern. Below is a quick look at the most prescribed groups.
| Class | Mechanism | Typical Drugs | Onset of Action | Common Side Effects | Key Contra‑indications |
|---|---|---|---|---|---|
| Selective Serotonin Reuptake Inhibitor (SSRI) blocks serotonin re‑uptake, raising its synaptic levels | Inhibits serotonin transporter (SERT) | Fluoxetine, Sertraline, Citalopram, Escitalopram | 2-4 weeks | nausea, sexual dysfunction, insomnia, headache | Concurrent MAOI use, severe liver disease |
| Serotonin‑Norepinephrine Reuptake Inhibitor (SNRI) blocks re‑uptake of both serotonin and norepinephrine | Inhibits SERT and NET | Venlafaxine, Duloxetine, Desvenlafaxine | 3-5 weeks | dry mouth, increased blood pressure, dizziness | Uncontrolled hypertension, recent MAOI therapy |
| Tricyclic Antidepressant (TCA) blocks re‑uptake of serotonin and norepinephrine, also affects histamine and acetylcholine receptors | Inhibits SERT, NET; anticholinergic activity | Amitriptyline, Nortriptyline, Imipramine | 3-6 weeks | constipation, weight gain, cardiac arrhythmia, sedation | Recent myocardial infarction, glaucoma, urinary retention |
| Monoamine Oxidase Inhibitor (MAOI) inhibits the MAO enzyme, preventing breakdown of serotonin, norepinephrine, and dopamine | Blocks MAO‑A and/or MAO‑B | Phenelzine, Tranylcypromine, Isocarboxazid | 4-6 weeks | hypertensive crisis with tyramine foods, orthostatic hypotension | Psychoactive drug use, certain antidepressant combinations |
| Atypical Antidepressants varied mechanisms not fitting other classes | Varies - e.g., bupropion blocks dopamine & norepinephrine re‑uptake | Bupropion, Mirtazapine, Trazodone | 2-4 weeks (bupropion), 4-6 weeks (mirtazapine) | insomnia (bupropion), weight gain (mirtazapine), dizziness | Seizure disorder (bupropion), severe hepatic impairment |
Choosing the Right Medication: What the Guidelines Say
Professional bodies such as the UK’s NICE National Institute for Health and Care Excellence, which publishes evidence‑based treatment pathways for mental health recommend a stepped approach:
- First‑line: Start with an SSRI unless contraindicated.
- Second‑line: If an SSRI fails after an adequate trial (usually 6-8 weeks at therapeutic dose), switch to another SSRI, an SNRI, or an atypical agent.
- Third‑line/complex cases: Consider TCAs, MAOIs, or augmentation strategies (adding lithium, antipsychotics, or psychotherapy).
Key points to remember during selection:
- Patient history: Past response, side‑effect tolerance, medical comorbidities.
- Drug interactions: Many antidepressants affect cytochrome P450 enzymes; review current meds.
- Lifestyle factors: Alcohol use, smoking, pregnancy status.
- Patient preference: Some avoid sexual side effects, others worry about weight gain.
Managing Side Effects and Safety Concerns
Side effects are the most common reason patients stop treatment early. Knowing what to expect and how to mitigate them improves adherence.
- Gastro‑intestinal upset: Take the medication with food, start at a low dose and titrate slowly.
- Sexual dysfunction: Consider dose reduction, switching to bupropion or a different SSRI, or using a “drug‑holiday” after consulting a clinician.
- Weight changes: Monitor weight monthly; lifestyle counseling can offset modest gains.
- Sleep disturbances: For insomnia, take the drug earlier in the day; for sedation, switch to morning dosing.
Serious safety concerns include:
- Suicide risk: The FDA black box warning alerts that antidepressants may increase suicidal thoughts in children, adolescents, and young adults applies mainly to the first few weeks; close monitoring is essential.
- Serotonin syndrome: Combine serotonergic agents (e.g., SSRIs + tramadol) only under strict medical supervision.
- Withdrawal (discontinuation) syndrome: Abrupt stop can cause dizziness, flu‑like symptoms, and electric‑shock sensations; taper gradually over weeks.
When Medication Isn't Enough: Integrating Psychotherapy and Lifestyle
Medication works best when paired with non‑pharmacologic strategies. Cognitive‑behavioral therapy (CBT) a structured, goal‑oriented psychotherapy that challenges negative thought patterns and interpersonal therapy are first‑line psychotherapies for MDD. Exercise, regular sleep, and a balanced diet also boost neurotransmitter function and can reduce the needed dose of medication.
For patients who cannot tolerate any drug class, psychotherapy alone or emerging treatments like transcranial magnetic stimulation (TMS) become viable alternatives.

Practical Checklist for Starting an Antidepressant
- Confirm diagnosis of Major Depressive Disorder using DSM‑5 or ICD‑10 criteria.
- Discuss treatment goals, expected timeline (4‑6 weeks for measurable improvement).
- Screen for contraindications (e.g., cardiac issues for TCAs, tyramine‑rich diet for MAOIs).
- Choose a first‑line agent (usually an SSRI) and set a starting dose.
- Schedule follow‑up at 2 weeks to check side effects, then at 6 weeks for efficacy.
- Educate about warning signs: worsening mood, suicidal thoughts, unusual agitation.
- Plan a taper schedule for future discontinuation if remission is achieved.
Frequently Asked Questions
How long does it take for an antidepressant to start working?
Most patients notice a subtle improvement in sleep or appetite within the first week, but a clinically meaningful reduction in depressive symptoms usually appears after 4‑6 weeks of consistent dosing.
Can I take an antidepressant with alcohol?
Occasional light drinking is generally tolerated, but heavy alcohol can worsen depression, interfere with medication metabolism, and increase side‑effects like sedation. Discuss any alcohol use with your prescriber.
What is the difference between an SSRI and a SNRI?
Both block serotonin re‑uptake, but SNRIs also inhibit norepinephrine re‑uptake, which can help with pain and low energy but may raise blood pressure in some people.
Are antidepressants addictive?
They do not produce a classic “high” or craving, but the brain can adapt to their presence. That’s why a gradual taper is recommended to avoid withdrawal symptoms.
What should I do if I experience severe side effects?
Contact your prescriber right away. In many cases the dose can be lowered or the drug switched without losing therapeutic benefit.
Can antidepressants be used during pregnancy?
Some SSRIs are considered relatively safe, but each case needs a risk‑benefit evaluation with an obstetrician and psychiatrist, especially in the first trimester.
Next Steps If You’re Starting Treatment
1. Write down any current medications, supplements, and health conditions.
2. Schedule a baseline appointment with a prescriber who can explain dosing and set up follow‑up.
3. Keep a simple mood diary: note sleep, appetite, energy, and any side effects each day.
4. Reach out to a trusted friend or family member to share your treatment plan - social support improves outcomes.
5. If you notice worsening mood or thoughts of self‑harm, call your GP, go to A&E, or dial emergency services immediately.
Understanding how antidepressant medications fit into the broader picture of treating Major Depressive Disorder empowers you to make informed choices, stick with therapy long enough to see benefits, and adjust safely when needed. With the right drug, a supportive therapist, and a healthy lifestyle, most people achieve significant relief and can get back to a fulfilling life.
