Imagine your kidneys are like fine coffee filters. They let waste and extra water out, but keep all the good stuff-protein, blood cells, electrolytes-inside your body. Now imagine your immune system, the very thing meant to protect you, starts shooting at those filters. That’s glomerulonephritis. It’s not just a kidney problem. It’s an inside job: your own defenses turning against the tiny structures that keep your blood clean.
What Exactly Gets Damaged?
The glomeruli are the filters. Each kidney has about a million of them. They’re made of three layers: the endothelial cells lining the blood vessels, the basement membrane that acts like a mesh, and the podocytes-special cells that wrap around the capillaries like octopus arms. These podocytes are the gatekeepers. They have tiny foot-like projections that interlock, forming gaps just big enough for water and waste to pass through, but too small for protein or red blood cells. When glomerulonephritis hits, something goes wrong with the immune system. Antibodies or complement proteins (part of your body’s first-line defense) build up in or around the glomeruli. This triggers inflammation. The filters swell, leak, and eventually scar. You don’t feel it at first. But over time, you start losing protein in your urine, your blood pressure climbs, and your ankles swell.Two Main Ways It Shows Up
Glomerulonephritis doesn’t present the same way for everyone. It usually falls into one of two syndromes. Nephritic syndrome means your filters are inflamed and damaged, but not completely broken. Blood leaks through-so you see red or cola-colored urine. Your kidneys can’t handle fluid well, so you get high blood pressure and swelling. Creatinine levels rise, meaning your kidneys aren’t filtering as well. This is common in post-strep infections in kids. In fact, about 15% of acute kidney inflammation in children starts after a sore throat or skin infection. Most recover fully within two months. Nephrotic syndrome is worse. The filters are so damaged that they leak massive amounts of protein-over 3.5 grams a day. Your blood protein drops below 3.0 g/dL. Your liver tries to compensate by making more cholesterol, so your LDL soars past 160 mg/dL. Fluid pools in your legs, belly, and around your eyes. You feel tired, heavy, and constantly bloated. This is typical in IgA nephropathy and lupus nephritis.The Big Players: Types of Glomerulonephritis
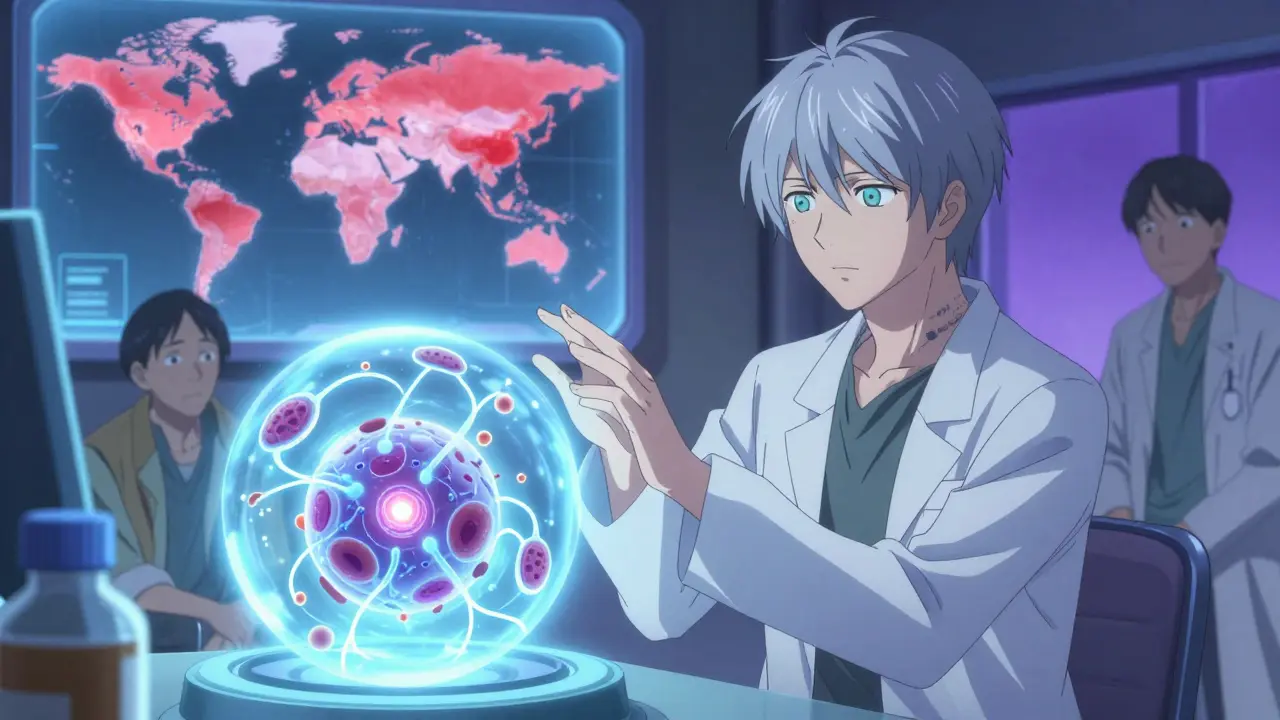
Not all glomerulonephritis is the same. The immune attack has different targets. IgA nephropathy is the most common form worldwide. It happens when IgA antibodies-normally fighting infections in your throat and gut-clump together and get stuck in the glomeruli. In North America, it affects about 2.5 people per 100,000 each year. In East Asia, it’s even more common-4 per 100,000. About 20-40% of people with this condition slowly lose kidney function over 20 years. Lupus nephritis affects half to two-thirds of people with systemic lupus erythematosus (SLE). Your immune system makes antibodies that attack your own tissues, and your kidneys are a prime target. With modern treatment, 70-80% of patients keep their kidney function after 10 years. Without it? The numbers drop fast. C3 glomerulonephritis (C3G) is rarer but more mysterious. Here, the complement system-your body’s automatic alarm system-goes haywire. C3 proteins build up in the glomeruli at 3 to 5 times normal levels. About 60-70% of C3G cases involve an autoantibody called C3 nephritic factor (C3NeF) that tricks the system into overactivating. It’s like your immune system has a stuck accelerator. Immune complex-mediated MPGN involves immune complexes (antibody + antigen clumps) lodging in the glomeruli. Biopsies show dense deposits under the electron microscope in 95% of cases. It’s often linked to chronic infections like hepatitis or autoimmune conditions.Why Diagnosis Takes So Long
Most people don’t realize they have glomerulonephritis until symptoms are obvious. Fatigue? Common. Swelling? Maybe you ate too much salt. Blood in urine? You assume it’s a UTI. The average time to diagnosis is over four months. Nearly a third of patients see three or more doctors before getting the right answer. Why? Because there’s no simple blood test. You need a kidney biopsy. A biopsy is invasive. There’s a 3-5% risk of bleeding. It’s not fun. But it’s the only way to tell the difference between IgA nephropathy, C3G, or lupus nephritis. And that matters-because treatment changes completely based on the type. Interpreting the biopsy? That’s a specialist’s job. Nephropathologists spend 5 to 7 years training just to read these slides accurately. One misread, and you get the wrong treatment.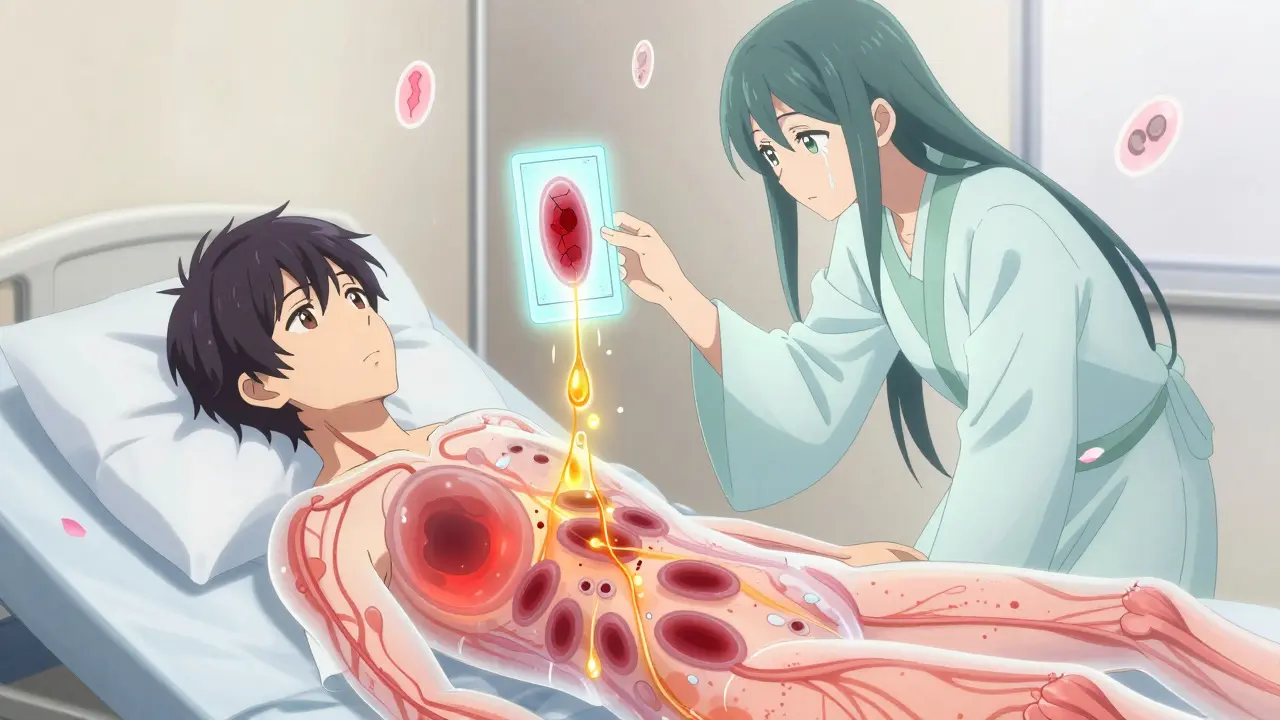
Current Treatments: Steroids and Their Costs
The go-to treatment for decades has been corticosteroids-like prednisone. They calm the immune system. About 60-80% of patients respond at first. But here’s the catch: side effects are brutal. - 72% gain weight rapidly - 35% get serious infections - 28% lose bone density, leading to fractures One patient on a support forum said prednisone caused two broken vertebrae in 18 months. Another said the swelling made her feel like she was “living in a balloon.” Steroids don’t fix the root problem. They just suppress everything-good and bad. That’s why 30-50% of patients relapse or don’t respond at all, according to the 2023 NEPTUNE study.What’s New? Targeted Therapies
The future of glomerulonephritis isn’t about blanket suppression. It’s about precision. For C3G, drugs like eculizumab and iptacopan block specific parts of the complement system. Iptacopan, approved for breakthrough therapy by the FDA in early 2023, cut proteinuria by 52% in trials. That’s huge. But there’s a problem: cost. Eculizumab runs about $500,000 per year. Not every hospital can afford it. Not every patient can access it. In low-income countries, patients have 90% less access to these drugs than those in the U.S. or Europe. Even in wealthy nations, insurance battles delay treatment for months. New guidelines from KDIGO (2023) say: try standard therapy for at least six months before jumping to these expensive drugs. But for some, six months is too long.The Podocyte: The Silent Victim
Podocytes don’t regenerate well. Once they’re damaged, they’re gone. That’s why proteinuria persists even after inflammation is controlled. Experts like Dr. Laura Barisoni at the University of Miami say the next big breakthrough will be therapies that don’t just stop the attack-but help podocytes heal. Imagine a treatment that doesn’t just calm the immune system, but rebuilds the filter. Some early research is looking at stem cell signals and growth factors that might trigger podocyte repair. It’s still experimental. But for patients who’ve spent years on dialysis, it’s the only hope that feels real.